221x Filetype XLSX File size 0.04 MB Source: iati.fcdo.gov.uk
Sheet 1: Goal and Purpose
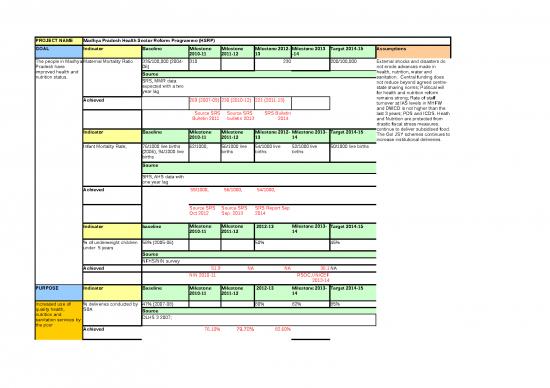
| PROJECT NAME | Madhya Pradesh Health Sector Reform Programme (HSRP) | |||||||
| GOAL | Indicator | Baseline | Milestone 2010-11 | Milestone 2011-12 | Milestone 2012-13 | Milestone 2013 -14 | Target 2014-15 | Assumptions |
| The people in Madhya Pradesh have improved health and nutrition status. | Maternal Mortality Ratio | 335/100,000 (2004-06) | 310 | 230 | 200/100,000 | External shocks and disasters do not erode advances made in health, nutrition, water and sanitation. Central funding does not reduce beyond agreed centre-state sharing norms; Political will for health and nutrition reform remains strong; Rate of staff turnover at IAS levels in MHFW and DWCD is not higher than the last 3 years; PDS and ICDS. Heath and Nutrition are protected from drastic fiscal stress measures. continue to deliver subsidised food. The GoI JSY schemes continues to increase institutional deliveries. | ||
| Source | ||||||||
| SRS, MMR data expected with a two year lag | ||||||||
| Achieved | 269 (2007-09) | 230 (2010-12) | 221 (2011-13) | |||||
| Source SRS Bulletin 2011 | Source SRS bulletin 2013 | SRS Bulletin 2014 | ||||||
| Indicator | Baseline | Milestone 2010-11 | Milestone 2011-12 | Milestone 2012-13 | Milestone 2013-14 | Target 2014-15 | ||
| Infant Mortality Rate, | 76/1000 live births (2006), 94/1000 live births | 62/1000, | 56/1000 live births | 54/1000 live births | 52/1000 live births | 50/1000 live births | ||
| Source | ||||||||
| SRS, AHS data with one year lag | ||||||||
| Achieved | 59/1000, | 56/1000, | 54/1000, | |||||
| Source SRS Oct 2012 | Source SRS Sep 2013 | SRS Report Sep 2014 | ||||||
| Indicator | baseline | Milestone 2010-11 | Milestone 2011-12 | 2012-13 | Milestone 2013-14 | Target 2014-15 | ||
| % of underweight children under 5 years | 58% (2005-06) | 50% | 45% | |||||
| Source | ||||||||
| NFHS/NIN survey | ||||||||
| Achieved | 51.9 | NA | NA | 36.1 | NA | |||
| NIN 2010-11 | RSOC,UNICEF 2013-14 | |||||||
| PURPOSE | Indicator | Baseline | Milestone 2010-11 | Milestone 2011-12 | 2012-13 | Milestone 2013-14 | Target 2014-15 | |
| Increased use of quality health, nutrition and sanitation services by the poor | % deliveries conducted by SBA | 47% (2007-08) | 80% | 82% | 85% | |||
| Source | ||||||||
| DLHS 3 2007; | ||||||||
| Achieved | 76.10% | 79.70% | 82.60% | |||||
| Source AHS | Source AHS | Source AHS | ||||||
| Indicator | Baseline | Milestone 2010-11 | Milestone 2011-12 | 2012-13 | Milestone 2013-14 | Target 2014-15 | ||
| % children with full immunisation | 36% | 42% | 46% | 50% | 54% | 58% | ||
| Source | ||||||||
| DLHS 3 -2007 | ||||||||
| Achieved | 54.90% | 59.70% | 66.40% | |||||
| Source AHS | Source AHS | Source AHS | ||||||
| Indicator | Baseline 2007-08 | Milestone 2010-11 | Milestone 2011-12 | Target 2012-13 | Milestone 2013-14 | Target 2014-15 | ||
| Percentage of children a. breast fed within an hour of birth; b. exclusively breast fed till six months. |
a. 43 % b. 31% |
a.55%, b.40%; |
a. 65%, b. 50%; |
|||||
| Source - DLHS 3 -2007 | ||||||||
| Achieved | a. 61.5 % b.36.8% | a. 65 % b.39.7% | a.66.8 % b.41.5% | |||||
| Source AHS | Source AHS | Source AHS | ||||||
| Indicator | Baseline | Milestone 2010-11 | Milestone 2011-12 | 2012-13 | Milestone 2013-14 | Target 2014-15 | ||
| Women receiving three ANC visits | 34.00% | 60% | 70% | 80% | ||||
| Source DLHS 3-2007 | ||||||||
| Achieved | 68.10% | 70.70% | 71.7% | |||||
| Source AHS | Source AHS | Source AHS | ||||||
| Indicator | Baseline + year | Milestone2010-11 | 2011-12 | 2012-13 | Milestone 2013-14 | Target 2014-15 | ||
| Percentage of women 15-49 yrs using modern methods of contraception | 53.0% | 56% | 58% | 60% | ||||
| Achieved | 57% | 59.30% | 59% | NA | ||||
| Source AHS | Source AHS | Source AHS | ||||||
| Source: DLHS 2008, AHS, DLHS 2013 | ||||||||
| INPUTS (£) | DFID (£) | State Govt (£) | Total (£) | DFID SHARE (%) | ||||
| GBP 120 m (between 2007/8 and 2015) | GBP 2500 m (Estimated budget of DHFW over 2007 and 15) GBP 1600 m is estimated budget for DWCD/ICDS over 2007-15 | GBP 4100 m (between 2007 and 15) | less than 2% of the total health and nutrition budget | |||||
| INPUTS (HR) | DFID (FTEs) | |||||||
| 1.5 | ||||||||
| OUTPUT 1 | Indicator | Baseline | Milestone 2012-13 | Milestone 2013-14 | Target 2014-2015 | Assumption |
| Quality public health and nutrition services available in underserved districts. | Indicator | 2007-08 | Milestone 2012-13 | Milestone 2013-14 | Target 2014-2015 | Quality of Care improves with better training, supervision and mentoring support. Reduced vacancies of doctors, nurses and specialists in remote districts.Integration of health and nutrition services improves uptake of both. If the quality and quantity of public health services are enhanced poor people will seek care. Regular weighing of young children according to new WHO growth norms as used as an entry point for improved breastfeeding counselling, IYCF practises and referrals to health services. All three factors of cconvergence: staff training, district level oversight and community management - will have an impact on child malnutrition to differing degrees |
| Functional quality assurance systems for Cemonc and Bemonc and delivery points. | Quality Monitoring framework designed and implementation started in 13 focus districts. Bimonthly quality monitoring done for 10 CEmONCs and 20 BEmONCs and Actions taken reports shared with govt. | QAC monitoring fully functional in 16 focus districts. QI inputs to 60 high load delivery points and bimonthly actions taken report. Functional facility based performance monitoring using QA MIS | Institutionalised systems for scale up of NQAS Road map and Supportive supervision for QI under implementation, being monitored by SQAC. 30 district and block hospitals have certified MMW and Compliance report on gaps identified for MMW across 50 districts. Direct QI inputs to 200 health facilities using NQAS in 16 focus districts. Quality implementation of RMNCH+A strategy in 17 High priority districts for supportive supervision and quality improvements at 450 delivery points and community centers (GAK and VHNDs). Scale up Skill labs to 4 divisions. |
|||
| Source | ||||||
| RCH JRM reports, NRHM CRM data, MIS, State Govt reports, Meeting minutes and TAST reports | ||||||
| Achieved :QAC set up in 14 districts.Quality monitoring done in 10 districts. | Achieved : (a).QAC functional across 16 TAST district and state quality assurance committee is also functional. (b).QI inputs have been provided for 90 high load delivery points. (c). Functional facility based performance monitoring using QA MIS has been acheived. | Achieved | ||||
| Improved Quality of community based integrated health and nutrition services. | Session on VHND incorporated into VHSC Training module. NGOs contracted in 16 districts to strengthen VHNDs: Trainings and VHND Quality monitoring started in atleast 10 districts. TAST support in 16 district to help implement ICDS district plans 2012 -13. ABM district plans for 2013 -14 finalised. ABM staff recruited and trained. CMAM approach approved by steering committee - roll out started | VHND quality monitoring and microplanning in 16 focus districts by TAST, NGOs, VHSCs and MGCAs. Direct VHND support to 1000 villages. District ABM/ICDS plans being implemented and monitored in 16 TAST districts. 350 AWC assessments and supervision every quarter for improved quality of nutrition services. 50 model AWC centers set up in select districts. | Gram arogya kendra (including VHND) supportive supervision and functionality improvements in 16 focus districts by TAST and State govt monitors in rest 34 districts. Comprehensive ASHA website functional to monitor ASHA performance, GAK, VHND, and VHSNC. Set up 50 model AWCs in 16 focus districts • Institutionalise QI process under ICDS Mission • Implementation and evaluation support for Suposhan phase 2• Training reforms policy framework to strengthen MLTCs and AWTCs included in ICDS Mission PIP |
|||
| Partially achieved :VHND quality monitoring in place in 5 districts.CMAM approach has been submitted for approval.State nutrition mission (ABM) started and funds allocated & staff recruited at state level.Ffive district facilitators have been placed in sagar division. | Achieved Quality Monitoring and microplanning of VHND in 16 districts. (b).Over acheivement;direct VHND support in 1340 villages so far. (c) Assessment of 350 AWCs and supervision acheived. d).Set up 50 model AWCs in 16 focus districts is partially acheived.As GOI approval is awaited. | All Achieved | ||||
| Source: Go MP reports, ICDS MIS, NIN survey, Studies, NRHM MIS | ||||||
| C | RISK RATING | |||||
| IMPACT WEIGHT= 0.25 | Medium | |||||
| DFID (£) | Govt (£) | |||||
| £30m | ||||||
| DFID (FTEs) | ||||||
| OUTPUT 2 | Indicator | Milestone 2011-12 | Milestone 2012-13 | Milestone 2013-14 | Target 2014-15 | Assumption | |||
| Improved quality of Human Resource Management in Health Sector | Better HR database informs rational deployment of human resources | Development of Doctors' database | Regular updation and quarterly analysis of doctors database to plan rational deployment. Doctors database web-enabled and put in public domain. | Quarterly analysis of doctors data base with evidence of use of HR analysis and rational deployment. Comprehensive HR database for all health staff designed and piloted. | HR database systems designed and functional to cover Doctors and nurses. HRMIS data regularly updated and analysed to take transfer decisions. | Supply of qualified staff improves across the country. HR planning unit headed by PS, established and staffed, and becomes a lead advisory agency on strategic HR issues. |
|||
| MP TAST Review Reports / GoMP Documents | |||||||||
| Achieved. | Achieved. HR database management information system (HRDMIS) has been designed by DFID TA team and updated regularly. | (a).Quarterly analysis of doctors data base has been achieved. (b).Partially achieved :Software developed and data updation for 60% nurses has been achieved. | All Achieved | ||||||
| Indicator | Milestone 2011-12 | Milestone 2012-13 | Milestone 2013-14 | Target 2014-15 | |||||
| HR Policy and Strategy developed along with departmental capacity augmentation | HR Cell established & staffed. Comprehensive HR policy developed for DH&FW | HR cell undertakes regular HR analysis, and supports recruitment and training planning. | • Restructuring of NHM structure and HR cell functions included. • SHRC Structure and functions designed and approved, funds allocated. • A new cadre of Hospital Administration at state and district levels to free up the time of medical/clinical staff from administrative jobs. • State and Divisional level Nursing re-organization designed and approved |
||||||
| Partially achieved: HR Cell established & staffed.But there is still scope to improvise the comprehensive HR policies. | All Achieved | All Achieved | |||||||
| MPTAST reports and GoMP documents | |||||||||
| IMPACT WEIGHTING | 0.2 | RISK RATING | |||||||
| High | |||||||||
| INPUTS (£) | DFID (£) | DFID SHARE (%) | |||||||
| 12m | |||||||||
| INPUTS (HR) | DFID (FTEs) | ||||||||
| 0.25 | |||||||||
no reviews yet
Please Login to review.