226x Filetype XLS File size 0.16 MB Source: assets.publishing.service.gov.uk
Sheet 1: Service Performance
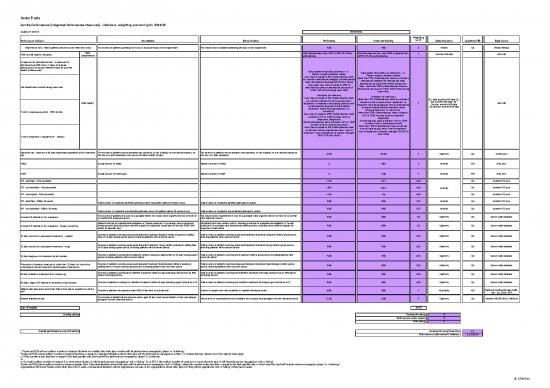
| Acute Trusts | ||||||||||||||||||
| Service Performance (Integrated Performance Measures) - Indicators, weighting and scoring for 2011/12 | ||||||||||||||||||
| Quality of service | Thresholds | |||||||||||||||||
| Performance Indicator | Numerator | Denominator | Performing | Under-performing | Weighting for PF | Data frequency | Quarterly/YTD | Data Source | ||||||||||
| Total time in A&E - 95% of patients should be seen within four hours | The number of patients spending four hours or less in all types of A&E department | The total number of patients attending all types of A&E department | 95% | 94% | 1 | Weekly | QA | Weekly SitReps | ||||||||||
| A&E clinical quality indicators | Data Completeness | HES attendances within 90 to 110% of SitRep attendances | HES attendances less than 80% or greater than 120% of SitRep attendances | 1 | Monthly HES data | A&E HES | ||||||||||||
| Unplanned re-attendance rate - Unplanned re-attendance at A&E within 7 days of original attendance (including if referred back by another health professional) | Data Quality | Data quality thresholds achieved – i.e. Patient Impact indicators (rates) Less than or equal to 5% of attendances have an unknown attendance category (re-attendance rate); attendance disposal (left without being seen rate); less than or equal to 10% of attendances have an attendance disposal of “other” (left without being seen rate); Indicators of timeliness Less than or equal to 5% of attendances have an unknown duration (time to assessment, departure, or treatment (excluding patients with an attendance disposal of leave before treatment, leave refusing treatment, or unknown)); Less than or equal to 25% of attendances have a duration of 0 or 1439 minutes (time to treatment, departure) Not all attendances have a duration of 0 or 1439 minutes (time to initial assessment) Less than or equal to 5% of attendances have an arrival, time of initial assessment, time of treatment, time of departure of exactly midnight (00:00 24 hour clock) |
Data quality thresholds not achieved – i.e. Patient Impact indicators (rates) More than 5% of attendances have an unknown attendance category (re-attendance rate); attendance disposal (left without being seen rate); more than 10% of attendances have an attendance disposal of “other” (left without being seen rate); Indicators of timeliness More than 5% of attendances have an unknown duration (time to assessment, departure, or treatment (excluding patients with an attendance disposal of leave before treatment, leave refusing treatment, or unknown)); More than 25% of attendances have a duration of 0 or 1439 minutes (time to treatment, departure) All attendances have a duration of 0 or 1439 minutes (time to initial assessment) More than 5% of attendances have an arrival, time of initial assessment, time of treatment, time of departure of exactly midnight (00:00 24 hour clock) |
1 | Q1: April monthly HES data Q2 : July monthly HES data Q3 : October monthly HES data Q4: January monthly HES data |
A&E HES | ||||||||||||
| Left department without being seen rate | ||||||||||||||||||
| Time to initial assessment - 95th centile | ||||||||||||||||||
| Time to treatment in department - median | ||||||||||||||||||
| Cancelled ops - breaches of 28 days readmission guarantee as % of cancelled ops | The number of patients whose operation was cancelled, by the hospital, for non-clinical reasons, on the day of or after admission, who were not treated within 28 days | The number of patients whose operation was cancelled, by the hospital, for non-clinical reasons on the day of or after admission | 5.0% | 15.0% | 1 | Quarterly | QA | QMCO, prov | ||||||||||
| MRSA | Actual number of MRSA | Planned number of MRSA | 0 | >1SD* | 1 | Monthly | YTD | HPA, prov | ||||||||||
| C Diff | Actual number of C Diff cases | Planned number of C Diff | 0 | >1SD | 1 | Monthly | YTD | HPA, prov | ||||||||||
| RTT - admitted - 95th percentile | <=23 | >27.7 | 0.50 | Monthly | QA | monthly RTT, prov | ||||||||||||
| RTT - non-admitted - 95th percentile | <18.3 | ≥18.3 | 0.50 | QA | monthly RTT, prov | |||||||||||||
| RTT - incomplete - 95th percentile | <=28 | >36 | 0.50 | QA | monthly RTT, prov | |||||||||||||
| RTT - admitted - 90% in 18 weeks | Total number of completed admitted pathways where the patient waited 18 weeks or less | Total number of completed admitted pathways in quarter | 90% | 85% | 0.75 | Monthly | QA | monthly RTT, prov | ||||||||||
| RTT - non-admitted - 95% in 18 weeks | Total number of completed non-admitted pathways where the patient waited 18 weeks or less | Total number of completed non-admitted pathways in quarter | 95% | 90% | 0.75 | Monthly | QA | monthly RTT, prov | ||||||||||
| 2 week GP referral to 1st outpatient | The number of patients first seen by a specialist within two weeks when urgently referred by their GP or dentist with suspected cancer | The total number of patients first seen by a specialist when urgently referred by their GP or dentist with suspected cancer | 93% | 88% | 0.5 | Quarterly | QA | Cancer waits database | ||||||||||
| 2 week GP referral to 1st outpatient - breast symptoms | Patients referred for evaluation/investigation of “breast symptoms” by a primary care professional during a period (excluding those referred urgently for suspected breast cancer) who are FIRST SEEN within 14 calendar days | All patients first seen within a period following a referral for evaluation/investigation of “breast symptoms” by a primary care professional within a period, excluding those referred urgently for suspected breast cancer | 93% | 88% | 0.5 | Quarterly | QA | Cancer waits database | ||||||||||
| 31 day second or subsequent treatment - surgery | Number of patients receiving subsequent/adjuvant treatment (surgery) within a maximum waiting time of 31-days during a given period, including patients with recurrent cancer | Total number of patients receiving subsequent/adjuvant treatment (surgery) within a given period, including patients with recurrent cancer | 94% | 89% | 0.25 | Quarterly | QA | Cancer waits database | ||||||||||
| 31 day second or subsequent treatment - drug | Number of patients receiving subsequent/adjuvant treatment (drug) within a maximum waiting time of 31-days during a given period, including patients with recurrent cancer. | Total number of patients receiving subsequent/adjuvant treatment (drug) within a given period, including patients with recurrent cancer | 98% | 93% | 0.25 | Quarterly | QA | Cancer waits database | ||||||||||
| 31 day diagnosis to treatment for all cancers | Number of patients receiving first treatment within a maximum waiting time of 31-days during a given period, including patients with recurrent cancer | Total number of patients receiving first treatment within a given period, including patients with recurrent cancer | 96% | 91% | 0.25 | Quarterly | QA | Cancer waits database | ||||||||||
| Proportion of patients waiting no more than 31 days for second or subsequent cancer treatment (radiotherapy treatments) | Number of patients receiving subsequent/adjuvant treatment (radiotherapy) within a maximum waiting time of 31-days during a given period, including patients with recurrent cancer. | Total number of patients receiving subsequent/adjuvant treatment (radiotherapy) within a given period, including patients with recurrent cancer. | 94% | 89% | 0.25 | Quarterly | QA | Cancer waits database | ||||||||||
| 62 day referral to treatment from screening | Number of patients receiving first definitive treatment within 62-days following referral from an NHS Cancer Screening Service | Total number of patients receiving first definitive treatment following referral from an NHS Cancer Screening Service | 90% | 85% | 0.50 | Quarterly | QA | Cancer waits database | ||||||||||
| 62 days urgent GP referral to treatment of all cancers | Number of patients receiving first definitive treatment within 62-days following urgent referral by a GP | Total number of patients receiving first definitive treatment following urgent referral by a GP | 85% | 80% | 0.50 | Quarterly | QA | Cancer waits database | ||||||||||
| Patients that have spent more than 90% of their stay in hospital on a stroke unit | Number of patients who spend at least 90% of their time on a stroke unit | Number of people who were admitted to hospital following a stroke | 60% | 30% | 1 | Quarterly | QA | National Sentinel Stroke Audit, Apr - Jun 2010, RCP | ||||||||||
| Delayed transfers of care | The number of patients (acute and non-acute, aged 18 and over) whose transfer of care was delayed, averaged over the reference period | The number of consultant and non-consultant led occupied beds averaged over the reference period | 3.5% | 5.0% | 1 | Quarterly | QA | Monthly MSITDT, KH03, QNCBeds | ||||||||||
| Sum of weights | 14.00 | |||||||||||||||||
| Scoring values | Underperforming: | 0 | ||||||||||||||||
| Performance under review: | 2 | |||||||||||||||||
| Performing: | 3 | |||||||||||||||||
| Overall performance score threshold | Underperforming if less than | 2.1 | ||||||||||||||||
| Performance under review if between | 2.1 and 2.4 | |||||||||||||||||
| * Trusts and PCTs with an outturn number of cases at the level of or better than their plan number will be performance-managed as ‘green’ or ‘achieving’. Trusts and PCTs whose outturn number of cases is less than or equal to 1 standard deviation above their plan will be performance-managed as ‘amber’ or ‘underachieving’, unless one of two special rules apply: a. if this number is also less than or equal to the best quartile rate, the trust will be performance-managed as ‘green’ or ‘achieving’ or b. if a trust's outturn number of cases is 5 or more above its plan, it will be performance-managed as 'red' or 'failing'. For a PCT, if the outturn number of cases is 6 or more above its plan, it will be performance-managed as 'red' or 'failing'. Trusts and PCTs whose outturn number of cases is greater than 1 standard deviation above their plan will be performance-managed as ‘red’ or ‘failing’, unless this number is also less than or equal to the best quartile rate, in which case the trust will be performance-managed as ‘green’ or ‘achieving’. Organisations (PCTs and Trusts) where their plan is for 0 cases, one standard deviation will be regarded as one case, ie for organisations where their plan is 0, they will be regarded as 'red' or 'failing' if they have 2 cases. |
||||||||||||||||||
| Due to in-year changes to A&E scoring, A&E CQIs will be used for data quality at a national level, not performance, thorughout 2011/12. More detail on data coverage is given below: | ||||||||||||||||||
| Data Coverage | ||||||||||||||||||
| ● Strep data re published at http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/WeeklySituationReports/index/htm | ||||||||||||||||||
| ● Sitrep data are collected on a weekly basis, rather than a calendar-monthly basis (with the exception of Aug-Oct 2011 Sitrep data); Weekly Sitrep data have been scaled using the simple quotient of "Number of days in the calendar month"/number of days in Sireps weeks falling within the month" (e.g. 5 weeks of sitrep data were attributed to the month of January 2011 therefore the scaling factor used to apportion sitrep data into a calendar month was 31/35 | ||||||||||||||||||
| ● An indication is given of whether organisations A&E HES attendance volumes are within 0% or 20% of the volumes reported in Sireps | ||||||||||||||||||
| ● Organisations that report sata to SitReps but not to A&E HES are flagged as "no data" | ||||||||||||||||||
| ● Organisations are flagged as "no data" if they report data to A&E HES but the attendance category for all attendances is unknown | ||||||||||||||||||
| ● It is recognised that coverage may vary for different types of department within the same organisation even if the total number of attendances in A&E HES is similar to the total number of attendance in SitReps for an organisation | ||||||||||||||||||
| ● It should be noted that some organisations report more data to A&E HES than SitReps, which may inflate estimates of coverage levels | ||||||||||||||||||
| ● Some organisations report data to A&E HES but not SitReps; this is generally due to cases where services have been reconfigured or renamed in one dataset and these changes have not yet been made in the other data set | ||||||||||||||||||
| Finance | |||||||||||||||||||
| SCORING | |||||||||||||||||||
| Criteria | Metric | Weight (%) | Performaing (3) | Performance under review (2) | Underperforming (1) | ||||||||||||||
| Initial Planning | Planned Outturn as a proportion of Turnover | Formula for organisations with a planned operating breakeven or surplus | Formula for organisations with a planned operating deficit | 5 | 5 | Planned operating breakeven or surplus that is either equal to or at variance to SHA expectations by no more than 3% of income. | Any operating deficit less than 2% of income OR an operating surplus/breakeven that is at variance to SHA expectations by more than 3% of planned income. | Operating deficit more than or equal to 2% of planned income | |||||||||||
| SHA expected operating surplus or breakeven - planned operating surplus or breakeven | x 100 | Planned operating deficit | x 100 | ||||||||||||||||
| Planned Income | Planned Income | ||||||||||||||||||
| Year to Date | YTD Operating Performance | Formula for organisations with a YTD actual operating breakeven or surplus | Formula for organisations with a YTD actual operating deficit | 25 | 20 | YTD operating breakeven or surplus that is either equal to or at variance to plan by no more than 3% of forecast income. | Any operating deficit less than 2% of income OR an operating surplus/breakeven that is at variance to plan by more than 3% of forecast income. | Operating deficit more than or equal to 2% of forecast income | |||||||||||
| YTD planned operating breakeven/ surplus/deficit - YTD actual operating breakeven or surplus | x 100 | YTD operating deficit | x 100 | ||||||||||||||||
| Forecast Income | Forecast Income | ||||||||||||||||||
| YTD EBITDA | YTD EBITDA | x 100 | 5 | Year to date EBITDA equal to or greater than 5% of actual year to date income | Year to date EBITDA equal to or greater than 1% but less than 5% of year to date income | Year to date EBITDA less than 1% of actual year to date income. | |||||||||||||
| Actual YTD Income | |||||||||||||||||||
| Forecast Outturn | Forecast Operating Performance | Formula for organisations with a forecast operating breakeven or surplus | Formula to be used for organisations with a forecast operating deficit | 40 | 20 | Forecast operating breakeven or surplus that is either equal to or at variance to plan by no more than 3% of forecast income. | Any operating deficit less than 2% of income OR an operating surplus/breakeven that is at variance to plan by more than 3% of income. | Operating deficit more than or equal to 2% of income | |||||||||||
| Planned operating breakeven/ surplus/deficit - Forecast operating breakeven or surplus | x100 | Forecast operating deficit | x100 | ||||||||||||||||
| Forecast Income | Forecast Income | ||||||||||||||||||
| Forecast EBITDA | Forecast EBITDA | x 100 | 5 | Forecast EBITDA equal to or greater than 5% of forecast income. | Forecast EBITDA equal to or greater than 1% but less than 5% of forecast income. | Forecast EBITDA less than 1% of forecast income. | |||||||||||||
| Forecast Income | |||||||||||||||||||
| Rate of Change in Forecast Surplus or Deficit. | (Current period forecast surplus/deficit) - (Prior period forecast surplus/deficit) | x 100 | 15 | Forecasting an operating deficit with a movement less than 2% of forecast income OR an operating surplus movement more than 3% of income. | Forecasting an operating deficit with a movement of greater than 2% of forecast income. | ||||||||||||||
| Forecast Income | |||||||||||||||||||
| Underlying Financial Position | Underlying Position % | Underlying Breakeven/Surplus/Deficit | x 100 | 10 | 5 | An underlying deficit that is less than 2% of underlying income. | An underlying deficit that is greater than 2% of underlying income | ||||||||||||
| Underlying Income | |||||||||||||||||||
| EBITDA Margin (%) | Underlying EBITDA | x 100 | 5 | Underlying EBITDA equal to or greater than 5% of underlying income | Underlying EBITDA less than 5% but equal to or greater than 1% of underlying income | Underlying EBITDA less than 1% of underlying income | |||||||||||||
| Underlying Income | |||||||||||||||||||
| Finance Processes & Balance Sheet Efficiency | Better Payment Practice Code Value % | Value of ALL Bills paid within target | x 100 | 20 | 2.5 | 95% or more of the value of NHS and Non NHS bills are paid within 30days | Less than 95% but more than or equal to 60% of the value of NHS and Non NHS bills are paid within 30days | Less than 60% of the value of NHS and Non NHS bills are paid within 30 days | |||||||||||
| Value of ALL Bills paid within the year | |||||||||||||||||||
| Better Payment Practice Code Volume % | Volume of ALL Bills paid within target | x 100 | 2.5 | 95% or more of the volume of NHS and Non NHS bills are paid within 30days | Less than 95% but more than or equal to 60% of the volume of NHS and Non NHS bills are paid within 30days | Less than 60% of the volume of NHS and Non NHS bills are paid within 30 days | |||||||||||||
| Volume of ALL Bills paid within the year | |||||||||||||||||||
| Current Ratio | Current Assets | 5 | Current Ratio is equal to or greater than 1. | Current ratio is anything less than 1 and greater than or equal to 0.5 | A current ratio of less than 0.5 | ||||||||||||||
| Current Liabilities | |||||||||||||||||||
| Receivable Days | Receivable as at current period | x365 | 5 | Receivable days less than or equal to 30 days | Debtor days greater than 30 and less than or equal to 60 days | Debtor days greater than 60 | |||||||||||||
| Forecast Income | |||||||||||||||||||
| Payable Days | Payable as at current period | x365 | 5 | Creditor days less than or equal to 30 | Creditor days greater than 30 and less than or equal to 60 days | Creditor days greater than 60 | |||||||||||||
| Total Expenditure | |||||||||||||||||||
| *Operating Position = Retained Surplus/Breakeven/deficit less impairments | 100 | 100 | |||||||||||||||||
| Over-riding Rules: | All organisations are subject to the following over riding rules: | ||||||||||||||||||
| 1.Forecasting a year end operational deficit that is less than or equal to plan - max Performance under review (2) | |||||||||||||||||||
| 2.Forecasting a year end operational deficit that is greater than plan - max Underperforming (1) | |||||||||||||||||||
| 3.Year to date operational deficit adverse to plan by more than 2% of full year income or £5m whichever is the smaller - max Performance under review (2) | |||||||||||||||||||
| 4.Unable to make any loan repayment due to insufficient cash – max Underperforming (1) | |||||||||||||||||||
no reviews yet
Please Login to review.