180x Filetype PDF File size 0.26 MB Source: www.binasss.sa.cr
In-flight Medical Emergencies
Jocelyn S. Hu, MD, Bayne-Jones Army Community Hospital, Fort Polk, Louisiana
Jordan K. Smith, MD, Christus Mother Frances Hospital, Sulphur Springs, Texas
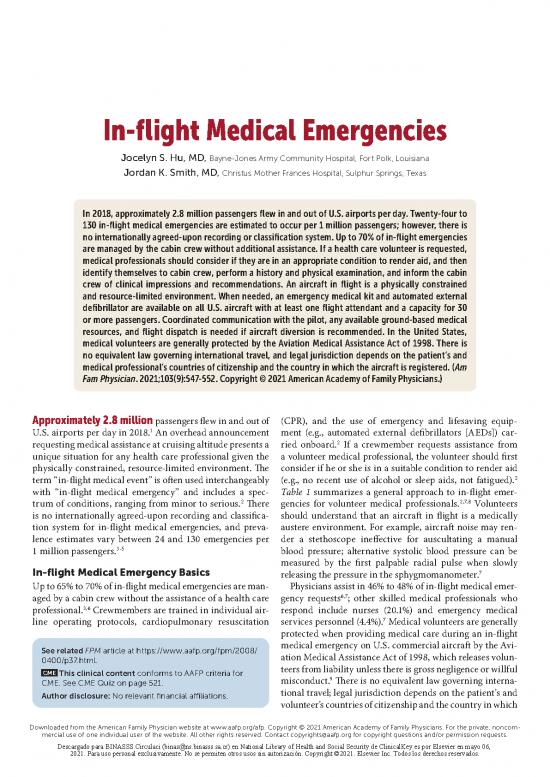
In 2018, approximately 2.8 million passengers flew in and out of U.S. airports per day. Twenty-four to
130 in-flight medical emergencies are estimated to occur per 1 million passengers; h owever, there is
no internationally agreed-upon recording or classification system. Up to 70% of in-flight emergencies
are managed by the cabin crew without additional assistance. If a health care volunteer is requested,
medical professionals should consider if they are in an appropriate condition to render aid, and then
identify themselves to cabin crew, perform a history and physical examination, and inform the cabin
crew of clinical impressions and recommendations. An aircraft in flight is a physically constrained
and resource-limited environment. When needed, an emergency medical kit and automated external
defibrillator are available on all U.S. aircraft with at least one flight attendant and a capacity for 30
or more passengers. Coordinated communication with the pilot, any available ground-based medical
resources, and flight dispatch is needed if aircraft diversion is recommended. In the United States,
medical volunteers are generally protected by the Aviation Medical Assistance Act of 1998. There is
no equivalent law governing international travel, and legal jurisdiction depends on the patient’s and
medical professional’s countries of citizenship and the country in which the aircraft is registered. (Am
Fam Physician. 2021;103(9):547-552. Copyright © 2021 American Academy of Family Physicians.)
Approximately 2.8 million passengers flew in and out of (CPR), and the use of emergency and lifesaving equip-
1
U.S. airports per day in 2018. An overhead announcement ment (e.g., automated external defibrillators [AEDs]) car-
2
requesting medical assistance at cruising altitude presents a ried onboard. If a crewmember requests assistance from
unique situation for any health care professional given the a volunteer medical professional, the volunteer should first
physically constrained, resource-limited environment. The consider if he or she is in a suitable condition to render aid
2
term “in-flight medical event” is often used interchangeably (e.g., no recent use of alcohol or sleep aids, not fatigued).
with “in-flight medical emergency” and includes a spec- Table 1 summarizes a general approach to in-flight emer-
2 2,7,8
trum of conditions, ranging from minor to serious. There gencies for volunteer medical professionals. Volunteers
is no internationally agreed-upon recording and classifica- should understand that an aircraft in flight is a medically
tion system for in-flight medical emergencies, and preva- austere environment. For example, aircraft noise may ren-
lence estimates vary between 24 and 130 emergencies per der a stethoscope ineffective for auscultating a manual
1 million passengers.3-5 blood pressure; alternative systolic blood pressure can be
measured by the first palpable radial pulse when slowly
In-flight Medical Emergency Basics 7
releasing the pressure in the sphygmomanometer.
Up to 65% to 70% of in-flight medical emergencies are man- Physicians assist in 46% to 48% of in-flight medical emer-
6,7
aged by a cabin crew without the assistance of a health care gency requests ; other skilled medical professionals who
3,6
professional. Crewmembers are trained in individual air- respond include nurses (20.1%) and emergency medical
7
line operating protocols, cardiopulmonary resuscitation services personnel (4.4%). Medical volunteers are generally
protected when providing medical care during an in-flight
See related FPM article at https:// www.aafp.org/fpm/2008/ medical emergency on U.S. commercial aircraft by the Avi-
0400/p37.html. ation Medical Assistance Act of 1998, which releases volun-
CME teers from liability unless there is gross negligence or willful
This clinical content conforms to AAFP criteria for 9
CME. See CME Quiz on page 521. misconduct. There is no equivalent law governing interna-
Author disclosure: No relevant financial affiliations. tional travel; legal jurisdiction depends on the patient’s and
volunteer’s countries of citizenship and the country in which
Downloaded from the American Family Physician website at www.aafp.org/afp. Copyright © 2021 American Academy of Family Physicians. For the private, noncom-Downloaded from the American Family Physician website at www.aafp.org/afp. Copyright © 2021 American Academy of Family Physicians. For the private, noncom-
◆
May 1, 2021 Volume 103, Number 9 www.aafp.org/afp American Family Physician 547
mercial use of one individual user of the website. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.mercial use of one individual user of the website. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.
Descargado para BINASSS Circulaci (binas@ns.binasss.sa.cr) en National Library of Health and Social Security de ClinicalKey.es por Elsevier en mayo 06,
2021. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2021. Elsevier Inc. Todos los derechos reservados.
IN-FLIGHT MEDICAL EMERGENCIES
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Evidence
Clinical recommendation rating Comments
Medical volunteers onboard the aircraft should consider ethical factors (e.g., appro- C Expert opinion in the absence
priate physical and mental condition to render aid, practice within scope of expertise) of clinical trials
in response to a request for medical assistance from a cabin crewmember.2,7,8
Medical volunteers onboard the aircraft should render aid with confidence that C Existing legislation and legal
the overall personal legal risk is small unless there is gross negligence or willful precedence in the absence of
9,10,13,14,16,17 clinical trials
misconduct.
Aircraft diversion recommendations should be made by the pilot, flight dispatch, C Expert opinion and consensus
cabin crew, medical volunteers, and ground-based medical support; t he decision to guideline in the absence of
divert is ultimately up to the pilot.7,22 clinical trials
For the initial management of syncope or near-syncope, the passenger should be C Expert opinion and usual
placed in a supine position with legs elevated, be given supplemental oxygen, and practice in the absence of
have blood glucose level checked.7,17,22 clinical trials
For the initial management of dyspnea, pulse oximetry should be checked, supple- C Expert opinion and usual
mental oxygen given, and an inhaled bronchodilator administered as indicated.17,22 practice in the absence of
clinical trials
Initial management of cardiovascular symptoms such as chest pain or cardiac arrest C Expert opinion, usual practice,
should include obtaining vital signs, providing supplemental oxygen, administering and consensus guidelines in the
aspirin and nitroglycerin, and using basic life support techniques.7,17,22 absence of clinical trials
A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-
oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to https:// www.aafp.
org/afpsort.
the aircraft is registered.8,10-13 The United States,
TABLE 1 England, and Canada do not mandate physicians
13-15
In-flight Medical Emergency Treatment Approach to render emergency medical services in flight,
for Volunteer Medical Professionals but a legal obligation to assist exists in Australia
10,14
and many other European countries. Experts
Identify yourself and state your medical qualifications. The airline may in aviation medicine support the use of medi-
require proof of credentials (e.g., business card, licensure documents). cal volunteers for in-flight medical emergencies
16,17
Perform as much of a complete history as possible. because the overall personal legal risk is small.
This may require an interpreter, involvement from family members, There has yet to be a U.S. case heard in court
or other nearby passengers. against a physician-passenger providing medical
10,14
Identify high-risk symptoms (e.g., chest pain, shortness of breath, care during an in-flight medical emergency.
focal neurologic deficits).
Onboard Medical Equipment
Obtain vital signs and perform an appropriate physical examination. The Federal Aviation Administration (FAA)
Inform the cabin crew of your clinical impression and recommendations. has mandated that certain medical supplies be
Initiate ground-based consultation if not already initiated by the flight crew. 18
available on U.S. commercial aircraft (Table 2) ;
The airline may require consultation before using the emergency similarly, the European Union Aviation Safety
medical kit. Agency and International Civil Aviation Organi-
Aircraft diversion and ground-based medical assistance require zation have established minimum recommenda-
coordination with the ground-based consultant and pilot. 18-20
tions for emergency medical kit contents. The
Administer supplemental oxygen or use an automated external defibrilla- FAA requires an AED on aircraft with at least one
tor as indicated. flight attendant and a capacity for 30 or more pas-
Document the clinical presentation and care rendered; the airline may 18
sengers. No such mandate exists for European
have specific forms to complete. airlines; h owever, many carry an AED onboard.21
Note: Do not attempt to practice beyond your level of expertise, but remember Non-U.S. airlines may carry additional con-
that your assistance is valuable and better than that of a nonmedical professional. 19,21
trolled substances for analgesia and sedation.
Information from references 2, 7, and 8. Some U.S. and international airlines have opted
to expand their emergency medical kits with
◆
548 American Family Physician www.aafp.org/afp Volume 103, Number 9 May 1, 2021
Descargado para BINASSS Circulaci (binas@ns.binasss.sa.cr) en National Library of Health and Social Security de ClinicalKey.es por Elsevier en mayo 06,
2021. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2021. Elsevier Inc. Todos los derechos reservados.
IN-FLIGHT MEDICAL EMERGENCIES
additional medications or equipment TABLE 2
19,22
(Table 3). If the desired item is not
available in the kit, the flight crew Federal Aviation Administration-Mandated Emergency
can make an overhead announce- Medical Kit Equipment and Medications
ment requesting the item from other
passengers. Equipment Medications
An anonymous survey of 12 Euro- Adhesive tape Antihistamine tablets, 25 mg
pean airlines that included full-service Alcohol sponges Antihistamine injectable, 50 mg
and low-cost carriers demonstrated a Cardiopulmonary resuscitation masks* Aspirin tablets, 325 mg
high degree of variability in emergency Intravenous line start kit with tubing Atropine, 0.5 mg
medical kit contents. None of the kits and Y-connectors Bronchodilator, inhaled
complied with International Civil Avi- Needles (18-, 20-, and 22-gauge) Dextrose, 50% per 50 mL, injectable
ation Organization recommendations; Oropharyngeal airways* Epinephrine 1: 1000, 1 mL, injectable
two were found to be insufficiently Protective nonpermeable gloves Epinephrine 1: 10,000, 2 mL, injectable
equipped for in-flight medical emer- Self-inflating manual resuscitation Lidocaine, 5 mL, 20 mg per mL,
23 device with masks*
gencies requiring acute care. Medical injectable
volunteers should know that these kits Sphygmomanometer Nitroglycerin tablets, 0.4 mg
generally are designed for adults and Stethoscope Nonnarcotic analgesic tablets, 325 mg
may not have basic airway equipment Syringes (5 mL, 10 mL) Saline solution, 500 mL
24 Tape scissors
and medication dosing for children.
Multiple medical organizations, Tourniquet
including the International Acad- Note: All airplanes with at least one flight attendant and a capacity for 30 or more passengers
emy of Aviation and Space Medicine, are required to have an automated external defibrillator.
American Osteopathic Association, *—Three sizes: child, small adult, and large adult or equivalent.
American College of Emergency Phy- Adapted from Federal Aviation Administration. Advisory circular 121-33B: e mergency med-
https:// www.faa.gov/
sicians, and American Medical Asso- ical equipment. January 12, 2006. Accessed October 11, 2019.
ciation have requested the addition of documentlibrary/media/advisory_circular/ac121-33b.pdf
pulse oximeters, naloxone, antiemet-
ics, and sedatives among other items.21
However, the FAA-mandated emergency medical kit is Aircraft Diversion
usually sufficient for initiating treatment for most in-flight Approximately 4% to 7% of in-flight medical emergencies
7
medical emergencies. result in aircraft diversion, with the most common reasons
being cardiac arrest (57.9%), cardiac symptoms (18.4%),
Ground-Based Medical Resources 7,22
obstetric emergencies (18.0%), and possible stroke (16.4%).
The FAA does not require in-flight consultation with The decision to divert an aircraft is made by the pilot in con-
ground-based medical support, but many airlines contract junction with flight dispatch and recommendations from
6,7
with a third party to help manage medical emergencies. the cabin crew, medical volunteers, and ground-based medi-
The pilot is notified by a crewmember when a medical emer- cal support. Factors include patient preference (or by proxy a
gency occurs. The pilot then establishes contact with the family member), weather, fuel load, airport capabilities, and
7,22
ground-based medical group and the airline operations cen- proximity of medical resources to specific airports.
ter to determine the best course of action. Board-certified
emergency physicians typically staff ground-based groups Considerations for Specific Conditions
7,8 SYNCOPE
and have additional training in aviation and telemedicine.
Crewmembers are often required to contact ground-based A review of 49,000 in-flight medical emergencies found
7
medical support before using the emergency medical kit. syncope or near-syncope to be the most common emer-
22
Communication is paramount because of the challenges gency category with a prevalence of 32.7%. Patients often
of radio interference and indirect patient contact. Ground- have initial mild bradycardia and hypotension, and may
based medical resources are involved in approximately 16 appear ill, pale, diaphoretic, or have a slightly altered men-
7
in-flight medical emergencies per 1 million passengers. tal status. The passenger should be placed in a supine or
There are no current studies on the effect of ground-based Trendelenburg position, which may require movement of
medical support on patient outcomes.22 the passenger into an aisle or galley with the legs elevated
◆
May 1, 2021 Volume 103, Number 9 www.aafp.org/afp American Family Physician 549
Descargado para BINASSS Circulaci (binas@ns.binasss.sa.cr) en National Library of Health and Social Security de ClinicalKey.es por Elsevier en mayo 06,
2021. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2021. Elsevier Inc. Todos los derechos reservados.
IN-FLIGHT MEDICAL EMERGENCIES
22
TABLE 3 or thrombosis, and toxic exposure. In a passen-
ger with dyspnea, pulse oximetry level should be
Expanded Emergency Medical Kit Equipment obtained, and supplemental oxygen administered
and Medications if oxygen saturation is less than 95%. If a passen-
ger uses 4 L per minute of supplemental oxygen or
Equipment Medications Medications more on the ground, the onboard oxygen supply
Children’s ventilation Amiodarone (continued) may not be sufficient to reverse hypoxia; therefore,
masks (additional sizes) Antacids Metoprolol 22
aircraft diversion may be required. Bronchodi-
Endotracheal tubes Dexamethasone Midazolam lators are available in emergency medical kits and
Foley catheter Diazepam (Valium) Naloxone should be administered for bronchospasm. If the
Glucometer Digoxin Ondansetron patient does not improve, ground-based medical
Laryngoscope Dimenhydrinate (Zofran) support should provide additional recommen-
Magill forceps Furosemide (Lasix) Prednisolone dations about the best use of available medical
Nasal cannula Prednisone 7
Glucagon resources given airline operational concerns.
Pulse oximeter Haloperidol Ranitidine
Sterile drapes (Zantac) CHEST PAIN
Heparin Scopolamine Chest pain or other cardiovascular symptoms
Suction catheters Loperamide (Imodium)
Suction pump Tramadol have a prevalence of 7% of in-flight medical
Meclizine (Antivert) emergencies and can be secondary to acute cor-
Thermometer Metoclopramide
Urine bag (Reglan) onary syndrome, anxiety, aortic dissection, mus-
culoskeletal pain, or pulmonary causes such as
Information from references 19 and 22. pulmonary embolus, bronchospasm, or pneumo-
22
thorax. Dyspepsia is often a diagnosis of exclu-
sion. Cardiac arrests are reported separately with
7
on a seat. Providing supplemental oxygen should be con- a prevalence of 0.2% of in-flight medical emergencies but
7,22
sidered, and the patient’s blood glucose level should be account for up to 86% of emergencies that result in death.
17
obtained with a finger stick device if available. If the pas- The initial assessment should include performing a focused
senger does not recover within 15 to 30 minutes of initial cardiovascular history and obtaining vital signs. If acute
interventions, contacting ground-based medical support coronary syndrome is suspected, aspirin and nitroglycerin
and recommending an aircraft diversion should be con- are typically included in FAA-mandated emergency medi-
sidered because of more serious causes for loss of con- cal kits. Chest pain that subsides with basic interventions is
sciousness such as acute coronary syndrome, arrhythmia, not usually caused by an acute ST-segment elevation myo-
22
hypoxia, pulmonary embolism or thrombosis, and stroke. cardial infarction, aortic dissection, or pulmonary embo-
Patients with persistent hypotension may need intravenous lism warranting diversion; h owever, the passenger should
fluids if oral intake is not tolerated. be offered transport to a hospital by emergency service per-
17
sonnel on landing.
DYSPNEA For a patient with suspected cardiac arrest (i.e., unre-
Dyspnea accounts for 10.1% of in-flight medical emergen- sponsive, not breathing or agonal gasps, no pulse), the pilot
22
cies. Cabin pressure is inversely proportional to the alti- and ground-based medical support should be notified and
tude of the aircraft, and aircraft cabins are not pressurized basic life support initiated, including high-quality CPR and
to sea level equivalent. Although the barometric pressure at use of an AED. Most aircraft will not have the capability
sea level corresponds to an arterial oxygen pressure of 95 to perform 12-lead electrocardiography. Epinephrine and
to 98 mm Hg, the barometric pressure at 8,000 ft (2,438 m) lidocaine are available in emergency medical kits for vol-
results in an arterial oxygen pressure of 55 to 56 mm Hg unteers comfortable with advanced life support algorithms
8,25
and a corresponding blood oxygen saturation of 90%. and can be administered per ground-based medical sup-
Most healthy travelers can compensate for this degree of port recommendations. CPR should be continued until
hypoxemia; passengers with known hypoxemia (i.e., resting one of the following occurs: return of spontaneous circu-
oxygen saturation less than 92% at sea level) are advised to lation; it becomes unsafe to continue CPR; a ll rescuers are
17
travel with portable oxygen. Causes for dyspnea include too exhausted to continue; the aircraft has landed, and care
asthma or chronic obstructive pulmonary disease, allergic is transferred to the ground-support medical team; o r the
reaction, pneumonia, pneumothorax, pulmonary embolism patient is presumed dead (i.e., CPR has been maintained for
◆
550 American Family Physician www.aafp.org/afp Volume 103, Number 9 May 1, 2021
Descargado para BINASSS Circulaci (binas@ns.binasss.sa.cr) en National Library of Health and Social Security de ClinicalKey.es por Elsevier en mayo 06,
2021. Para uso personal exclusivamente. No se permiten otros usos sin autorización. Copyright ©2021. Elsevier Inc. Todos los derechos reservados.
no reviews yet
Please Login to review.