299x Filetype XLSX File size 0.41 MB Source: www.macpac.gov
Sheet 1: Introduction
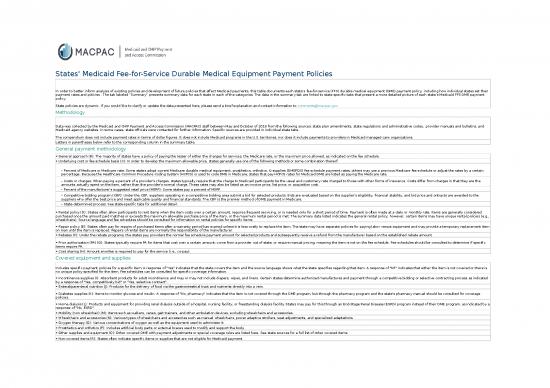
| States' Medicaid Fee-for-Service Durable Medical Equipment Payment Policies | ||||||||
| In order to better inform analysis of existing policies and development of future policies that affect Medicaid payments, this table documents each state’s fee-for-service (FFS) durable medical equipment (DME) payment policy, including how individual states set their payment rates and policies . The tab labeled “Summary” presents summary data for each state in each of the categories. The data in the summary tab are linked to state-specific tabs that present a more detailed picture of each state’s Medicaid FFS DME payment policy. State policies are dynamic. If you would like to clarify or update the data presented here, please send a brief explanation and contact information to comments@macpac.gov. |
||||||||
| Methodology | ||||||||
| Data was collected by the Medicaid and CHIP Payment and Access Commission (MACPAC) staff between May and October of 2018 from the following sources: state plan amendments, state regulations and administrative codes, provider manuals and bulletins, and Medicaid agency websites. In some cases, state officials were contacted for further information. Specific sources are provided in individual state tabs. The compendium does not include payment rates in terms of dollar figures. It does not include Medicaid programs in the U.S. territories, nor does it include payments to providers in Medicaid managed care organizations. |
||||||||
| Letters in parentheses below refer to the corresponding column in the summary table. | ||||||||
| General payment methodology | ||||||||
| • General approach (B): The majority of states have a policy of paying the lesser of either the charges for services, the Medicare rate, or the maximum price allowed, as indicated on the fee schedule. | ||||||||
| • Underlying cost or fee-schedule basis (C): In order to develop the maximum allowable price, states generally use one of the following methods or some combination thereof: | ||||||||
| – Percent of Medicare or Medicare rate: Some states adopt current Medicare durable medical equipment, prosthetics, orthotics, & supplies (DMEPOS) fee schedule payment rates, others may use a previous Medicare fee schedule or adjust the rates by a certain percentage. Because the Healthcare Common Procedure Coding System (HCPCS) is used to code DME in Medicare, states that pay HCPCS rates for Medicaid DME are listed as paying the Medicare rate. | ||||||||
| – Costs or charges: When paying a percent of a provider's charges, states typically require that the charge to Medicaid participants be the usual and customary rate charged to those with other forms of insurance. Costs differ from charges in that they are the amounts actually spent on the item, rather than the provider's normal charge. These rates may also be listed as an invoice price, list price, or acquisition cost. | ||||||||
| – Percent of the manufacturer’s suggested retail price (MSRP): Some states pay a percent of MSRP. | ||||||||
| – Competitive bidding program (CBP): Under the CBP, suppliers operating in a competitive bidding area submit a bid for selected products. Bids are evaluated based on the supplier’s eligibility, financial stability, and bid price and ontracts are awarded to the suppliers who offer the best price and meet applicable quality and financial standards. The CBP is the premier method of DME payment in Medicare. | ||||||||
| – State-determined process: See state-specific tabs for additional detail. | ||||||||
| • Rental policy (D): States often allow participants to rent items when the item costs over a certain amount, requires frequent servicing, or is needed only for a short period of time. Payment is often made at a daily or monthly rate. Items are generally considered purchased once the amount paid matches or exceeds the maximum allowable purchase price of the item, or the maximum rental period is met. The summary data listed indicates the general rental policy; however, certain items may have unique rental policies (e.g., wheelchairs). Source language and fee schedules should be consulted for information on rental policies for specific items. | ||||||||
| • Repair policy (E): States often pay for repairs of purchased items after a warranty period has expired unless it is less costly to replace the item. The state may have separate policies for paying labor versus equipment and may provide a temporary replacement item on loan until the item is replaced. Repairs of rental items are normally the responsibility of the manufacturer. | ||||||||
| • Rebates (F): Under the rebate programs, the states pay providers the normal fee schedule payment amount for selected products and subsequently receive a refund from the manufacturer based on the established rebate amount. | ||||||||
| • Prior authorization (PA) (G): States typically require PA for items that cost over a certain amount; come from a provider out of state; or require manual pricing, meaning the item is not on the fee schedule. Fee schedules should be consulted to determine if specific items require PA. | ||||||||
| • Cost sharing (H): Amount enrollee is required to pay for the service (i.e., co-pay). | ||||||||
| Covered equipment and supplies | ||||||||
| Includes specific payment policies for a specific item. A response of "Yes" indicates that the state covers the item and the source language shows what the state specifies regarding that item. A response of "NF" indicates that either the item is not covered or there is no unique policy specified for the item. Fee schedules can be consulted for specific coverage information. | ||||||||
| • Incontinence supplies (I): Absorbent products for adult incontinence and may or may not include diapers, wipes, and liners. Certain states determine authorized manufactures and payment through a competitive bidding or selective contracting process as indicated by a response of "Yes, competitively bid" or "Yes, selective contract". | ||||||||
| • Enteral/parenteral nutrition (J): Products for the delivery of food via the gastrointestinal tract and nutrients directly into a vein. | ||||||||
| • Diabetes supplies (K): Items to monitor glucose and insulin. A response of "No, pharmacy" indicates that the item is not covered through the DME program, but through the pharmacy program and the state's pharmacy manual should be consulted for coverage policies. | ||||||||
| • Home dialysis (L): Products and equipment for providing renal dialysis outside of a hospital, nursing facility, or freestanding dialysis facility. States may pay for this through an End-Stage Renal Disease (ESRD) program instead of their DME program, as indicated by a response of "No, ESRD". | ||||||||
| • Mobility (non wheelchair) (M): Items such as walkers, canes, gait trainers, and other ambulation devices, excluding wheelchairs and accessories. | ||||||||
| • Wheelchairs and accessories (N): Various types of wheelchairs and accessories such as manual wheelchairs, power adaptive strollers, seat adjustments, and specialized adaptations. | ||||||||
| • Oxygen therapy (O): Various concentrations of oxygen as well as the equipment used to administer it. | ||||||||
| • Prosthetics and orthotics (P): Includes artificial body parts or external braces used to modify and support the body. | ||||||||
| • Other supplies and equipment (Q): Other covered DME with payment adjustments or special coverage rules are listed here. See state sources for a full list of other covered items. | ||||||||
| • Non-covered items (R): States often indicate specific items or supplies that are not eligible for Medicaid payment. |
| Medicaid Durable Medical Equipment Fee-for-Service Payment Policies | |||||||||||||||||
| State | General | Covered supplies and equipment | |||||||||||||||
| General approach | Underlying cost or fee-schedule basis | Rental policy | Repair policy | Rebates | Prior authorization (PA) | Cost sharing | Incontinence supplies | Enteral/parenteral nutrition | Diabetes supplies | Home dialysis | Mobility (non wheelchair) | Wheelchairs and accessories | Oxygen therapy | Prosthetics and orthotics | Other supplies and equipment | Non-covered items | |
| Alabama | Medicare rate or state process | Medicare rate or state process | Covered for 90 days without PA, Covered for six months or more as rent-to-purchase |
Labor: covered up to three hours, Parts: covered at price plus 20 percent or maximum allowable |
NF | Certain items | Ranges from $0.65 to $3.90 | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Alaska | Lesser of charges or maximum allowable | Medicare rate or state process | Less than 30 days: paid daily rate, 30 days or more: paid 10 percent of purchase price per month |
Labor: up to $20 per 15 minutes, Parts: covered |
NF | Certain items, including rentals and special requests | NF | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Arizona | Included in inpatient or outpatient rate | NA | Covered if less costly than purchase price | Purchased items only | NF | Required for equipment over $300 or $500, required for supplies over $100, required for orthotics for adults | NF | Yes | NF | NF | NF | NF | NF | NF | NF | NF | Yes |
| Arkansas | Lesser of charges or maximum allowable | Percent of Medicare or percent of manufacturer charge | Covered up to 455 days, daily rate based on Medicare rate | Covered at 110 percent of cost, labor covered up to five hours per day | NF | Required for items over $1000, required for certain prosthetics | Ranges from 10 percent to 20 percent of maximum allowable, for those above 100 percent FPL | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| California | Lesser of charges, purchase price or maximum allowable | State process | Montly rate | Purchased items only | Yes | Required for items over $100 | NF | Yes | No, pharmacy | Yes | No, ESRD | Yes | Yes | Yes | Yes | Yes | Yes |
| Colorado | Lesser of charges or maximum allowable | Percent of MSRP, provider charge or percent of cost | Covered up to max rental period and purchase price, varies by item | Purchased items only | Yes | Certain items | $1 for certain items, children and pregnant women excluded | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | NF | NF |
| Connecticut | Lesser of charges or maximum allowable | Medicare rate or provider charge | Covered up to max rental period, varies by item | Purchased items only | NF | Certain items | None | NF | Yes | NF | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Delaware | Medicare rate or state process | Medicare rate or state process | Covered up to purchase price, monthly rate based on Medicare rate | Purchased items only, up to one month rental fee | NF | Certain items | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| District of Columbia | Lesser of charges or maximum allowable | State process | Covered up to six months or purchase price, monthly rate | Purchased items only, up to 75 percent of purchase price | NF | Certain items | NF | NF | Yes | Yes | NF | NF | Yes | Yes | NF | Yes | Yes |
| Florida | Lesser of competitive bidding rate or maximum allowable | Competitive bidding rate or percent of provider charge | Covered up to purchase price | Included in rate | NF | Certain items | NF | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Georgia | Lesser of percent of Medicare or charges | Percent of Medicare or provider charge | Covered up to 10 months, certain items continuously rented | Purchased items only, PA required | NF | Certain items, including items and repairs over $200, rentals and special requests | $3 for certain codes | No | Yes | No, pharmacy | NF | Yes | Yes | Yes | NF | Yes | Yes |
| Hawaii | Lesser of Medicare rate or charges | NF | Covered up to purchase price, certain items covered at Medicare rate | Purchased items only | NF | Certain items | NF | Yes | Yes | NF | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Idaho | Lesser of charges or maximum allowable | Percent of MSRP or percent of cost | Covered up to 10 months, monthly rate | Covered | NF | Required, with exceptions | NF | Yes | Yes | NF | NF | NF | Yes | Yes | Yes | Yes | Yes |
| Illinois | Lesser of charges or maximum allowable | Percent of Medicare, percent of cost or percent of MSRP | Covered up to 10 months or purchase price | Certain items may require PA, including wheelchair repairs over $400 | NF | Certain items, excluding items covered by Medicare | None | Yes | No, pharmacy | No, pharmacy | NF | NF | Yes | Yes | Yes | Yes | Yes |
| Indiana | Lesser of charges or maximum allowable | Medicare rate | Covered up to 15 months, required for items needing frequent servicing | Purchased items only | Diabetic supplies | Required, with exceptions | NF | Yes, competitively bid | Yes | Yes | No, ESRD | Yes | Yes | Yes | Yes | Yes | Yes |
| Iowa | Lesser of Medicare rate or maximum allowable | Medicare rate, percent of MSRP or percent of cost | Covered up to purchase price, max rental period varies by item | Purchased items only, up to two-thirds of replacement cost | Yes | Certain items | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kansas | Lesser of percent of MSRP, percent of cost or maximum allowable | Percent of MSRP or percent of cost | Covered up to six months, low cost items not covered | Purchased items only, up to 75 percent of replacement cost | NF | Certain items | Ranges from $0 to $3 | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Kentucky | Lesser of charges, purchase price or maximum allowable | Percent of manufacturer charge or provider charge | Covered up to 10 months, 10 percent of purchase price per month or 2.5 percent of purchase price per week | Purchased items only, labor covered at lesser of charge or maximum allowable | NF | Required for purchased items over $500 or rentals over 12 months | $4 | NF | Yes | No, pharmacy | NF | NF | Yes | Yes | Yes | NF | Yes |
| Louisiana | Lesser of charges or maximum allowable | Percent of Medicare, percent of MSRP or percent of provider charge | Covered short term if less costly than purchase price | Purchased items only, maintenance not covered | NF | Required | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Maine | Lesser of Medicare rate, charges or maximum allowable | Medicare rate, percent of MSRP or percent of cost | Covered up to 12 months, one-twelfth of purchase price | PA required for costs over $699 or 60 percent of replacement cost | Yes | Certain items, including items over $699, rentals, and prosthetics and orthotics | Ranges from $.50 to $3 per day for purchased items, $3 per month for rental items |
Yes, competitively bid | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Maryland | Lesser of charges or maximum allowable | Provider charge, percent of Medicare, percent of MSRP, or percent of wholesale cost | Covered at nine percent of Medicare rate or 10 percent of purchase price | Purchased items only, paid percent of MSRP or percent of wholesale cost, Labor: billed per 15 minutes |
NF | Certain items and certain clients, excluding prosthetics and orthotics | NF | Yes | Yes | NF | Yes | NF | NF | Yes | Yes | Yes | Yes |
| Massachusetts | Lesser of preferred provider rate, charges or maximum allowable | Medicare rate or percent of cost | Covered up to three months at 10 percent of purchase price, Covered up to 13 months at 75 percent of short term rental rate |
Purchased items only, loaner provided up to five days | NF | Certain items, including repairs over $1000 and clients with other insurance | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Michigan | Maximum allowable | State process | Covered up to 10 months or purchase price | Purchased items only, no loaner provided | NF | Special requests | NF | Yes, competitively bid | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Minnesota | Lesser of Medicare rate or charges | Medicare rate, percent of MSRP, percent of provider charge, percent of cost | Covered up to 13 months or purchase price | Purchased items only, PA required for costs over $400 with exceptions | NF | Certain items | NF | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Mississippi | Lesser of charges or maximum allowable | Percent of Medicare, percent of cost or percent of MSRP | Covered up to 10 months or purchase price | Purchased items only, up to 50 percent of replacement cost | NF | Certain items, excluding medical supplies except incontinence | Ranges from $0.50 to 3 | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Missouri | Lesser of charges or maximum allowable | State process | Covered up to purchase price | Purchased items only, up to 60 percent of replacement cost | NF | Certain items | None | Yes | Yes | No, pharmacy | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Montana | Lesser of charges or maximum allowable | Medicare rate or percent of provider charge | Covered up to 13 months, 10 percent of purchase price per month | Purchased items only, except rental items Medicare classifies as needing frequent servicing | NF | Certain items | $4 | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Nebraska | Lesser of charges or maximum allowable | NF | Covered up to 12 months or purchase price, Required for items costing $150 or more |
Purchased items only, up to 80 percent of purchase price | NF | Certain items, including items over $750 | $3 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Nevada | Lesser of charges or maximum allowable | Medicare rate, percent of MSRP, percent of provider charge, percent of cost | Covered up to purchase price | Covered for items under five years old | NF | Required, with exceptions | NF | Yes | Yes | No, pharmacy | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| New Hampshire | Lesser of Medicare rate or maximum allowable | Medicare rate or state process | Covered for certain items with two month trial period | Covered at lesser of charge, lowest accepted rate or maximum allowable | NF | Incontinence supplies only | NF | Yes, competitively bid | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| New Jersey | Lesser of percent of manufacturer charge, charges, percent of cost or maximum allowable | Percent of manufacturer charge, provider charge or percent of cost | Covered up to 10 months at 12 percent of purchase price for items over $100, Covered up to six months at 12 percent of purchase price for items $100 or less |
Labor: maximum hourly allowable, Parts: lesser of charge, price or maximum allowable |
NF | Certain items, including supplies over $100 and equipment over $300 | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| New Mexico | Lesser of charges or maximum allowable | Medicare rate | Covered up to 13 months, percent of cost up to purchase price | Purchased items only, replacements may require PA | NF | Certain items | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| New York | Lesser of charges or maximum allowable | Percent of provider charge or percent of cost | Required for items needing trial period up to purchase price, 10 percent of purchase price per month | Covered once per year, PA not required for prosthetic/orthotic repairs under 10 percent of cost | Diabetic supplies | Required | $1 | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| North Carolina | Lesser of charges or maximum allowable | Medicare rate | Covered up to 15 months or purchase price, monthly rate | Purchased items only, PA required | Diabetic supplies | Certain items | None | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| North Dakota | Lesser of charges or maximum allowable | Medicare rate or state process | Covered up to 12 months, PA required | Covered up to 75 percent of replacement, PA required | NF | Certain items, including items over $500 | None | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Ohio | Percent of Medicare or lesser of percent of manufacturer charge or percent of provider charge | Percent of Medicare, percent of manufacturer charge, percent of provider charge | Covered up to six months without PA, 10 percent of purchase price per month | Covered, no loaner provided | NF | Required for customized and used DME, and special requests | None | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Oklahoma | Lesser of charges or maximum allowable | Medicare rate or state process | Covered up to 13 months or purchase price, certain items continuously rented | Purchased items only, price includes loaner | NF | Special requests | NF | Yes | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes |
| Oregon | Lesser of MSRP, charges or maximum allowable | Percent of Medicare or state process | Covered up to purchase price | Purchased items only | Yes | Required for HCPCS level II codes | NF | Yes | NF | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Pennsylvania | Lesser of charges or maximum allowable | Medicare rate or provider charge | Covered up to six months without PA, monthly rate | Covered | NF | Required for items over $600 | Ranges from $.65 to $7.60 | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rhode Island | Lesser of charges or maximum allowable | Percent of MSRP, provider charge or percent of cost | Covered up to purchase price, monthly rate | Purchased items only | NF | Certain items | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| South Carolina | Lesser of charges or maximum allowable | Percent of MSRP or percent of cost | Covered up to 10 months, Limited rentals covered up to four months |
Purchased items only | NF | Certain items | $3.40 | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| South Dakota | Lesser of usual and customary charges, percent of charges or maximum allowable | Percent of provider charge | Covered up to six or 12 months or purchase price for items over $120 | Covered at lesser of charge or purchase price | NF | Certain items | Five percent of maximum allowable | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Tennessee | Lesser of competitive bidding rate, percent of Medicare, charges or maximum allowable | Competitive bidding rate, percent of Medicare or provider charge | Covered at 10 percent of purchase price, monthly rate | Covered at 80 percent of charges | NF | NF | NF | NF | NF | NF | NF | NF | NF | NF | NF | NF | NF |
| Texas | Lesser of charges or maximum allowable | Percent of Medicare, percent of cost or percent of MSRP | Coverage varies by item and client, up to purchase price | Purchased items only, labor included in cost | NF | Required, with exceptions | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Utah | Medicare rate or maximum allowable | Medicare rate or percent of manufacturer charge | Covered up to 12 months, certain items continuously rented | Purchased items only, PA required | NF | Certain items | NF | Yes | Yes | Yes | NF | NF | Yes | Yes | Yes | Yes | Yes |
| Vermont | Lesser of percent of MSRP, charges or percent of cost or maximum allowable | Percent of MSRP, provider charge or percent of cost | Covered short term, 10 percent of purchase price per month | Covered up to 50 percent of replacement cost | NF | Required, with exceptions | None | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Virginia | Percent of Medicare or maximum allowable | Percent of Medicare or percent of manufacturer charge | Covered short term up to purchase price, daily rate | Purchased items only, PA required for costs over allowed amount | NF | Certain items and certain clients | None | Yes, selective contract | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Washington | Lesser of Medicare rate, charges or maximum allowable | Medicare rate or state process | Daily rate, based on Medicare rate or percent of manufacturer price | Covered | NF | Certain items | NF | Yes | Yes | Yes | No, ESRD | Yes | Yes | Yes | Yes | Yes | Yes |
| West Virginia | Lesser of charges or maximum allowable | Medicare rate | Covered up to 10 months or purchase price | Covered at lesser of charge or maximum allowable | NF | Certain items, retrospective authorization available | NF | Yes | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Wisconsin | Lesser of charges or maximum allowable | State process | Covered for short term, PA required after trial period | PA required for costs over $150 total, or $84 for labor | NF | Certain items and special requests | Ranges from $0.50 to $3 | Yes, competitively bid | Yes | Yes | NF | Yes | Yes | Yes | Yes | Yes | Yes |
| Wyoming | Lesser of Medicare rate, charges or percent of cost | Medicare rate, provider charge or percent of cost | Covered up to 10 months or 100 days, daily or monthly rate | Labor: covered for certain services, Repairs: covered |
NF | Certain items and certain clients, conducted via contractor | NF | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Notes: MSRP is manufacturer's suggested retail price. NF is none found. NA is not applicable. PA is prior authorization. Source date reflects the effective dates of the policies where available, otherwise it reflects the date listed on the publication. Data collected by the Medicaid and CHIP Payment and Access Commission (MACPAC) between May and October 2018, from the following sources: state plan amendments, state regulations and administrative codes, provider manuals and bulletins, Medicaid agency websites, Medicaid agency fee schedules, and additional searches of key terms in Google. In some cases, states were contacted for further information. Please contact MACPAC at 202-350-2000 or comments@macpac.gov to report errors or changes. | |||||||||||||||||
| Medicaid Durable Medical Equipment (DME) Fee-for-Service Payment Policies—Alabama | |||||
| Back to Summary | |||||
| Key Elements | Summary data | Details | Sources and websites | Source date | Date last searched |
| General | |||||
| General approach | Medicare rate or state process | For DME items described in section 1861(n) of the Social Security Act, the pricing methodology is equal to the Medicare rate, and will be updated on an annual basis based on the January Medicare published rate. The agency’s fee schedule rate is in effect for services provided on or after May 1, 2018. All rates are published on the Medicaid Agency’s website (www.medicaid.alabama.gov). Except as otherwise noted in the plan, the Medicaid developed fee schedule rates are the same for both governmental and private providers. If no Medicare price is available, Medicaid will establish a price for supplies, appliances, and durable medical equipment using the manufacturer's generated invoice to determine provider's actual cost after all discounts are applied. Medicaid will reimburse provider at their actual cost after all discounts are applied, plus 20% markup. If documented invoices cannot be obtained, reimbursement will be based on the Manufacturer Suggested Retail Price (MSRP) minus 40%. Freight and delivery, evaluation and fitting charges are included in the markup percentage for specially constructed wheelchairs. |
Alabama state plan amendment, attachment 4.19-B, p. 7: http://www.medicaid.alabama.gov/content/9.0_Resources/9.8_State_Plan.aspx. | 5/1/2018 | 9/21/2018 |
| Underlying cost or fee-schedule basis | Medicare rate or state process | For DME items described in section 1861(n) of the Social Security Act, the pricing methodology is equal to the Medicare rate, and will be updated on an annual basis based on the January Medicare published rate. The agency’s fee schedule rate is in effect for services provided on or after May 1, 2018. If no Medicare price is available, Medicaid will establish a price for supplies, appliances, and DME using the manuafacturer's generated invoice to determine the provider's actual cost after all discounts are applied. Medicaid will reimburse provider at their actual cost after all discounts are applied, plus 20% markup. If documented invoices cannot be obtained, reimbursement will be based on the MSRP minus 40%. Freight and delivery, evaluation and fitting charges are included in the markup percentage for specially constructed wheelchairs. If no Medicare price is available, reimbursement rates established by Medicaid for EPSDT-referred wheelchair systems will be based on a Discount from MSRP. Providers are required to submit available MSRPs from three manufacturers for equipment appropriate for the individual's medical needs. Provider must document the nonavailability of required MSRPs to justify sending in three prices. The established rate will be based on the MSRP minus the following discounts: 1. Manual Wheelchair Systems - 20% discount from MSRP 2. Power Wheelchair Systems - 15% 3. Ancillary (add-on) products - 20% |
Alabama state plan amendment, attachment 4.19-B, p. 7: http://www.medicaid.alabama.gov/content/9.0_Resources/9.8_State_Plan.aspx. | 5/1/2018 | 9/21/2018 |
| Rental policy | Covered for 90 days without PA, Covered for six months or more as rent-to-purchase |
Short Term Rental Policy Standard DME items prescribed as medically necessary can be rented if needed on a short term basis. Short term is described as six months or less. Applicable procedure codes are indicated on the fee schedule with an RR for rental. Medicaid payment for short term rental will be made when the following documentation is submitted: 1. Written order or prescription documenting an estimated period of time (number of months) that the medical equipment will be needed, and 2. Documentation that establishes medical necessity for the short term rental. Initial approval will consist of up to 90 days only. If the recipient needs the equipment beyond the initial 90 day period, written documentation (including an additional PA) must be submitted that demonstrates continued medical necessity. If equipment continues to be medically necessary longer than six months, a capped rental to purchase will be established. Capped Rental to Purchase (requires PA) • Providers must submit a new PA request for the purchase of the item with previous rental payments deducted from the total purchase price of the item. • Providers will submit their claims with the purchase price that Medicaid shows on the approved PA request for the purchase of the item. • The requested dates of service on the new PA request for purchase of the item must not overlap with the dates of service on the PA request for the rental period of the item. Previous rental payments will be applied towards the total purchase price of the equipment. • Reimbursement will not exceed the total purchase price of the equipment. Providers should be aware of Medicaid policy regulating medical necessity for durable medical equipment. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.1: Definitions: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Repair policy | Labor: covered up to three hours, Parts: covered at price plus 20 percent or maximum allowable |
Repairs K0739 repair or no routine service for durable medical equipment other than oxygen equipment requiring the skill of a technician, labor component, per 15 minutes. Effective January 1, 2015, the RB Modifier for Repair(s) for all wheelchair (manual or power) accessory procedure codes will allow a DME repair not exceeding $1,000 per day to bypass the need for PA. This may expedite the repair process which will be beneficial to Medicaid recipients and providers. This process will not apply to recipient’s ages 0-20. This process will not override the current limitation audits for each of the procedure codes. For example, if the recipient has already received the yearly limit for a specific procedure code (e.g., 2 per calendar year), the provider will have to submit a PA for the repair even if it is less than the threshold amount of $1,000. Effective February 1, 2012, the allowable units for K0739 are 12 per repair. However, providers must continue to submit justification with the PA request when submitting claims for more than four units. The request will be reviewed by Medicaid or its designee. The PA letter, in the Analyst Remarks section, will state the total units approved. Replacement Replacement parts are reimbursed based on the procedure code and fee schedule pricing. In situations where there are no procedure codes or fee schedule reimbursement for the repair item(s), the provider must submit an itemized list of the needed repair items with invoice pricing for each item. Alabama Medicaid will reimburse for these repair items based on provider’s invoice price plus 20%. The reimbursement amount will be calculated based on the provider's final invoice, after all discounts have been applied. Providers should submit their usual and customary charges for the service. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.4: Warranty, maintenance, replacement, and delivery: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Rebates | NF | NF | See notes below | NA | 5/16/2018 |
| Prior authorization (PA) | Certain items | Certain DME requires prior authorization. Please refer to DME Fee Schedule on the Agency’s website (www.medicaid.alabama.gov) for an inclusive listing of DME items that require PA. Payment will not be made for these procedures unless the PA request is received within thirty calendar days after the service is provided. PA requests for DME, supplies and appliances must include medical records to support the medical necessity of the requested item(s). Checklists are not sufficient medical documentation. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.3: Prior authorization and referral requirements: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Cost sharing | Ranges from $0.65 to $3.90 | Medicaid recipients are required to pay and suppliers are required to collect the designated copay amount for the rental/purchase of services, supplies, appliances, and equipment, including crossovers. The copayment does not apply to services provided for pregnant women, recipients less than 18 years of age, emergencies, surgical fees, and family planning. Native American Indians that present an “active user letter” issued by Indian health Services (IHS) will be exempt from the Medicaid required copayment. Durable Medical Equipment, including crossovers $3.90 for items costing $50.01 or more $2.60 for items costing $25.01-$50.00 $1.30 for items costing $10.01-$25.00 Supplies and Appliances, including crossovers $3.90 for items costing $50.01 or more $2.60 for items costing $25.01-$50.00 $1.30 for items costing $10.01-$25.00 $0.65 for items costing $10.00 or less Iron Infusion Pump Repair $ 3.90 for each Prior Authorization (PA) Number |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.4: Cost-sharing (copayment): http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Covered supplies and equipment | |||||
| Incontinence supplies | Yes | Incontinence Products (Disposable Diapers) Medicaid will consider payment of disposable diapers when referred as medically necessary from an EPSDT screening and the criteria below are met: 1. Recipient must be at least 3 years old; 2. Patient must be non-ambulatory or minimally ambulatory; and 3. Patient must be medically at risk for skin breakdown, which is defined as meeting at least two of the following: a. Unable to control bowel or bladder functions, b. Unable to utilize regular toilet facilities due to medical condition c. Unable to physically turn self or reposition self, d. Unable to transfer self from bed to chair or wheelchair without assistance. Special Ostomy Supplies A4221 Special ostomy supplies should be submitted using procedure code A4421 with an SC modifier. Special ostomy supplies will be reimbursed at provider’s invoice price plus 20% and will pay from the approved price listed on the PA file. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Sections 14.2.25, 14.2.37: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Enteral/parenteral nutrition | Yes | Enteral Nutrition Equipment and Supplies Enteral nutrition equipment and supplies are covered for children under the age of 21 with an EPSDT Screening and Referral. Recipients age 21 and above (with noted limitations) qualify based on medical necessity and prior authorization when the following criteria are met: The recipient meets the following criteria for enteral nutrition: a. Recipient is < age 21 and record supports that > than 50 % of need is met by specialized nutrition; OR b. Recipient is > age 21 and record supports 100 % of need is met by specialized nutrition and provided by tube feedings AND must submit documentation from the attending physician to support that the recipient cannot tolerate bolus feeding and requires enteral nutrition by pump. Total Parenteral Nutrition (TPN) Pump and Supplies All Total Parenteral Nutrition (TPN) supplies are provided to Medicaid recipients based on medical necessity when the following criteria are met: 1. The recipient meets the criteria for total parenteral nutrition (TPN) a. Recipient < age 21 and record supports that > than 50 % of need is met by specialized nutrition, or b. Recipient > age 21 and record supports 100 % of need is met by specialized nutrition. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Sections 14.2.27, 14.2.28: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Diabetes supplies | Yes | Home blood glucose monitors, monitor replacement batteries, calibrator solution/chips, and spring powered lancet devices must be prescribed as medically necessary by the primary physician. Providers dispensing diabetic supplies must have the recipient’s prescription/order on file from the primary care physician. A valid prescription/order will contain the frequency for daily blood sugar testing. Providers must ensure that diabetic supplies are dispensed based on the daily frequency of blood sugar testing indicated on the recipient’s prescription/order. It is the provider’s responsibility to ensure that the recipient does not have an excessive supply of strips/lancets. If it is determined through provider audits that Medicaid has reimbursed the provider for excessive amounts of strips/lancets, the amount paid for the excessive supply will be recouped. Effective March 1, 2012, DME diabetic testing supplies claims billed for recipients with Gestational Diabetes must contain a diagnosis code in the range of 64880 through 64884 for ICD-9, O24410 through O24439 and O99810 through O99815 for ICD-10. Note: Recipients who were diagnosed with diabetes prior to the pregnancy are eligible to receive diabetic equipment/supplies. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.7: Insulin devices and supplies: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Home dialysis | NF | NF | See notes below | NA | 5/16/2018 |
| Mobility (non wheelchair) | Yes | A specialty walker is a tool for disabled children with special needs who may require additional support to maintain balance or stability while walking. Medicaid will cover specialty walkers for children under the age of 21 with an EPSDT referral. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.5: Walkers: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Wheelchairs and accessories | Yes | To qualify for Medicaid reimbursement of a wheelchair, the physician must prescribe the equipment as medically necessary for the recipient. The recipient must be essentially bed confined and must meet the following documented conditions: • The recipient must be essentially chair confined or bed/chair confined. • The wheelchair is expected to increase mobility and independence. Effective October 1, 2011, Medicaid’s Motorized/Power Wheelchair Assessment Form 384 must be completed with all prior authorization requests for Manual Wheelchairs with additional accessories for adults. This form must be completed an Alabama licensed Physical Therapist (PT) or Occupational Therapist (OT) who has experience and training in mobility evaluations and is employed by a Medicaid enrolled hospital outpatient department. Medicaid uses Medicare-based allowables for EPSDT-referred wheelchair systems. If no Medicare price is available, reimbursement rates established by Medicaid for EPSDT-referred wheelchair systems are based on a discount from Manufacturers Suggested Retail Price (MSRP) instead of a "cost-plus" basis. To qualify for Medicaid reimbursement of a low pressure equalization pad, the equipment must be prescribed as medically necessary for the recipient by the physician. These procedure codes require prior authorization. 14.2.37 Adaptive Strollers, Equipment and Accessories Adaptive strollers, equipment and accessories are covered items in the DME program for Medicaid eligible children under the age of 21 through the EPSDT program who meet criteria. Medicaid will reimburse providers at provider’s invoice price plus 20%. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.15: Wheelchairs: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Oxygen therapy | Yes | 14.2.17 Oxygen Oxygen therapy is a covered service for the entire Medicaid population based on medical necessity and requires prior authorization. e. Criteria for equipment reimbursement i. Oxygen concentrators will be considered for users requiring one or more tanks per month of compressed gas (stationary unit). Prior approval requests will automatically be subjected to a review to determine if a concentrator will be most cost effective. ii. Reimbursement will be made for portable O2 only in gaseous form. Medicaid will cover portable oxygen for limited uses such as physician visits or trips to the hospital. This must be stated as such on the medical necessity or prior approval request. Portable systems that are used on a standby basis only will not be approved. Only one portable system (E0431) consisting of one tank and up to four refills (E0443) per month will be approved based on a review of submitted medical justification. An example of justification for refills includes, but is not limited to, multiple weekly visits for radiation or chemotherapy. iii. E1392: A portable oxygen concentrator may be approved if the reimbursement is more cost effective than a tank and multiple refills. The portable oxygen concentrator must accommodate the oxygen flow rate prescribed for the recipient and the time needed for portable oxygen, e.g., medical appointments. • If a recipient requires more than one refill (E0443), the provider must submit justification as to why the portable concentrator does not meet recipient’s needs. If not documented, the recipient must be provided a portable concentrator. Medicaid will reimburse for only one stationary system. iv. For initial certification for oxygen the DME supplier, and its employees, may not perform the ABG study or oximetry analysis used to determine medical necessity. v. Effective January 1, 2005 for recertification for oxygen only following qualifying sleep study which allows for approval of nocturnal oxygen, the DME supplier may perform the oximetry analysis to determine continued medical necessity for recipients receiving nocturnal oxygen only. A printed download of the oximetry results must be submitted with a prior authorization request. Handwritten results will not be accepted. 14.2.18 Pulse Oximeter Pulse oximeters are a covered service for EPSDT eligible individuals who are already approved for supplemental home oxygen systems and whose blood saturation levels fluctuate, thus requiring continuous or intermittent monitoring to adjust oxygen delivery. 14.2.19 Pulse Oximeter Supplies Supplies for the Pulse Oximeter will only be paid for by Medicaid after completion of the ten month rental period. 14.2.20 Volume Ventilator The ventilator will be reimbursed as a monthly rental item. The monthly rental includes delivery, in-service for caregiver, maintenance, a backup ventilator, back up battery, all medically necessary supplies, and repairs and on call service as necessary. Recertification is required until the recipient no longer meets the criteria or the device is removed from the home. If the ventilator is no longer medically necessary (i.e., the criteria is no longer met) it will be returned to the supplier. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.17: Oxygen: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Prosthetics and orthotics | Yes | (A) Prosthetic Devices Reasonable, customary charges submitted by the vendor, not to exceed the amount payable under Title XVIII, Part B or the amount paid by the general public. The pricing methodology is 80% of the 2005 Medicare allowable amount as listed on the Alabama Supplies, Appliances, and DME Fee Schedule. The agency's fee schedule rate is in effect for services provided on or after October 1, 2014. (B) 14.2.31 Prosthetic, Orthotic and Pedorthic Devices Covered for Medicaid Recipients age 21 and above Prosthetic related supply codes are covered if a recipient is an amputee, has a prosthetic leg, and these supplies are necessary for the function of the prosthetic. Ankle-foot orthoses (AFO) and knee-ankle foot orthoses... and knee-ankle foot orthoses (KAFO) are covered for ambulatory recipients with weakness or deformity of the foot and ankle, which requires stabilization for medical reasons, and have the potential to benefit functionally. Knee-ankle foot orthoses (KAFO) are primarily covered for ambulatory recipients that require additional knee stability and would not benefit from the AFO. 14.2.33 External Breast Prostheses External breast prostheses following mastectomy for breast cancer are covered for all Medicaid-eligible recipients meeting the criteria. |
(A) Alabama state plan amendment, attachment 4.19-B, p. 4: http://www.medicaid.alabama.gov/content/9.0_Resources/9.8_State_Plan.aspx. (B) DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Sections 14.2.31—14.2.33: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. |
(A) 4/1/2017 (B) 4/1/2018 |
5/16/2018 |
| Other supplies and equipment | Yes | Respiratory suction pumps; hospital bed & accessories; pediatric bed/crib; power reducing support surfaces (related to mattresses); nebulizer; iron chelation therapy equipment; augmentative communication devices; Continuous Positive Airway Pressure (CPAP); Bilateral Positive Airway Pressure (BI-PAP) Device; Home Phototherapy; High Frequency Chest Wall Oscillation Air Pulse Generator System; Apnea Monitor; Home Infusion Therapy Services Equipment and Supplies; Controlled Dose Drug Inhalation System; Enuresis Alarm | DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Non-covered items | Yes | Medicaid does not cover the following types of items: • Items of a deluxe nature • Replacement of usable equipment • Items for use in hospitals, nursing facilities, or other institutions • Items for recipient’s/caregiver’s comfort or convenience • Items not listed as covered by Medicaid • Rental of equipment, with exceptions noted below: o For Medicaid recipient’s for six months or less. o Medicare crossovers o Certain intravenous therapy equipment o Short term use due to institutionalization o Short term use due to death of a recipient o DME items may be provided in Nursing Homes or other institutions for children through the EPSDT Program. o Medicaid recipients may be billed for items not covered by Medicaid Medicaid recipients may be billed for non-covered items and items covered by non-contract providers. |
DXC Technology, Alabama Medicaid provider manual, Chapter 14: Durable medical equipment, Section 14.2.2: Non-covered items and services: http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. | 4/1/2018 | 5/16/2018 |
| Notes: EPSDT is early and periodic screening, diagnosis, and treatment. NF is none found. NA is not applicable. Source date reflects the effective dates of the policies where available, otherwise it reflects the date listed on the publication. Data collected by MACPAC between May and October 2018, from the following sources: state plan amendments, state regulations and administrative codes, provider manuals and bulletins, Medicaid agency websites, Medicaid agency fee schedules, and additional searches of key terms in Google. In some cases, states were contacted for further information. Please contact MACPAC at 202-350-2000 or comments@macpac.gov to report errors or changes. | |||||
| Sources: Centers for Medicare & Medicaid Services (CMS), U.S. Department of Health and Human Services. 2018. Attachment 4.19-B to Alabama Medicaid state plan. June 13, 2018. Baltimore, MD: CMS. http://www.medicaid.alabama.gov/content/9.0_Resources/9.8_State_Plan.aspx. DXC technology. 2018. Chapter 14: Durable medical equipment. In Alabama Medicaid provider billing manual. April 2018. Montgomery, AL. http://medicaid.alabama.gov/content/Gated/7.6.1G_Provider_Manuals.aspx. |
|||||
no reviews yet
Please Login to review.