212x Filetype PDF File size 2.05 MB Source: pedclerk.bsd.uchicago.edu
JOURNALOF Learning files (Reprint)
Family Focus on infant food allergy
HEALTH CARE
Cow's milk protein allergy and other
food hypersensitivities in infants
Dr Carina Venter reviews the diagnosis and clinical picture. In the case of cow’s milk hyper-
sensitivity, for example, they may present with
management of food hypersensitivity, including cow’s immunoglobulin E (IgE)-mediated symptoms
such as urticaria or angiodema, and also with non-
milk protein allergy, in infants and young children IgE-mediated gastrointestinal symptoms includ-
ing food protein enteropathy or non-allergic FHS
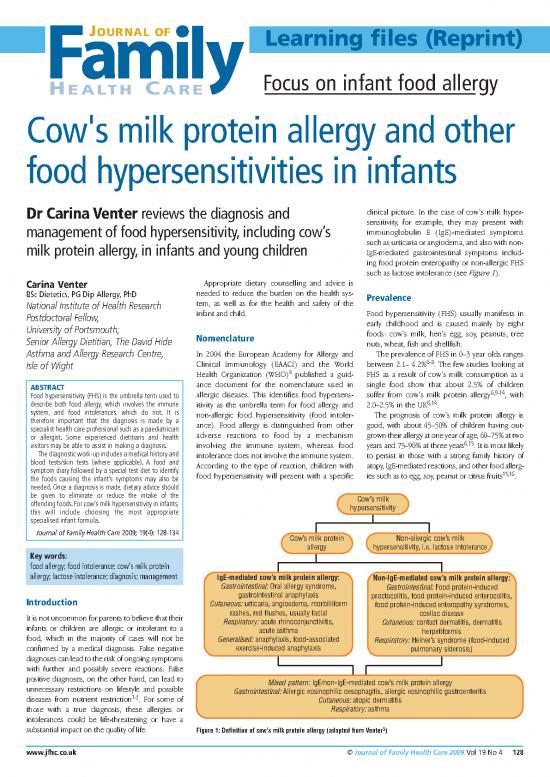
such as lactose intolerance (see Figure 1).
Carina Venter Appropriate dietary counselling and advice is
BSc Dietetics, PG Dip Allergy, PhD needed to reduce the burden on the health sys- Prevalence
National Institute of Health Research tem, as well as for the health and safety of the
Postdoctoral Fellow, infant and child. Food hypersensitivity (FHS) usually manifests in
University of Portsmouth; early childhood and is caused mainly by eight
Nomenclature foods: cow’s milk, hen’s egg, soy, peanuts, tree
Senior Allergy Dietitian, The David Hide nuts, wheat, fish and shellfish.
Asthma and Allergy Research Centre, In 2004 the European Academy for Allergy and The prevalence of FHS in 0–3 year olds ranges
6-8
Isle of Wight Clinical Immunology (EAACI) and the World between 2.1– 4.2% . The few studies looking at
Health Organization (WHO)4 published a guid- FHS as a result of cow’s milk consumption as a
ABSTRACT ance document for the nomenclature used in single food show that about 2.5% of children
Food hypersensitivity (FHS) is the umbrella term used to allergic diseases. This identifies food hypersens- suffer from cow’s milk protein allergy6,9-14, with
describe both food allergy, which involves the immune 2.0–2.5% in the UK6,14
itivity as the umbrella term for food allergy and .
system, and food intolerances, which do not. It is non-allergic food hypersensitivity (food intoler- The prognosis of cow’s milk protein allergy is
therefore important that the diagnosis is made by a ance). Food allergy is distinguished from other good, with about 45–50% of children having out-
specialist health care professional such as a paediatrician adverse reactions to food by a mechanism grown their allergy at one year of age, 60–75% at two
or allergist. Some experienced dietitians and health
6,15
visitors may be able to assist in making a diagnosis. involving the immune system, whereas food years and 75–90% at three years . It is most likely
The diagnostic work-up includes a medical history and intolerance does not involve the immune system. to persist in those with a strong family history of
blood tests/skin tests (where applicable). A food and According to the type of reaction, children with atopy, IgE-mediated reactions, and other food allerg-
symptom diary followed by a special test diet to identify food hypersensitivity will present with a specific ies such as to egg, soy, peanut or citrus fruits15,16.
the foods causing the infant’s symptoms may also be
needed. Once a diagnosis is made, dietary advice should
be given to eliminate or reduce the intake of the Cow’s milk
offending foods.For cow’s milk hypersensitivity in infants, hypersensitivity
this will include choosing the most appropriate
specialised infant formula.
Journal of Family Health Care 2009; 19(4): 128-134 Cow’s milk protein Non-allergic cow’s milk
allergy hypersensitivity, i.e. lactose intolerance
Key words:
food allergy; food intolerance; cow’s milk protein
allergy; lactose intolerance; diagnosis; management IgE-mediated cow’s milk protein allergy: Non-IgE-mediated cow’s milk protein allergy:
Gastrointestinal: Oral allergy syndrome, Gastrointestinal: Food protein-induced
Introduction gastrointestinal anaphylaxis proctocolitis, food protein-induced enterocolitis,
Cutaneous: urticaria, angioedema, morbilliform food protein-induced enteropathy syndromes,
It is not uncommon for parents to believe that their rashes, red flushes, usually facial coeliac disease
infants or children are allergic or intolerant to a Respiratory: acute rhinoconjunctivitis, Cutaneous: contact dermatitis, dermatitis
acute asthma herpetiformis
food, which in the majority of cases will not be Generalised: anaphylaxis, food-associated Respiratory: Heiner’s syndrome (food-induced
confirmed by a medical diagnosis. False negative exercise-induced anaphylaxis pulmonary siderosis)
diagnoses can lead to the risk of ongoing symptoms
with further and possibly severe reactions. False
positive diagnoses, on the other hand, can lead to Mixed pattern: IgE/non-IgE-mediated cow’s milk protein allergy
unnecessary restrictions on lifestyle and possible Gastrointestinal: Allergic eosinophilic oesophagitis, allergic eosinophilic gastroenteritis
diseases from nutrient restriction1-3
. For some of Cutaneous: atopic dermatitis
those with a true diagnosis, these allergies or Respiratory: asthma
intolerances could be life-threatening or have a
substantial impact on the quality of life. Figure 1: Definition of cow’s milk protein allergy (adapted from Venter5)
www.jfhc.co.uk ©Journal of Family Health Care 2009 Vol 19 No 4 128
Learning files
Very little data on the prevalence of lactose the diagnosis and management of FHS. (see below). There are now more specific clinical
intolerance is available, but it is estimated that decision measures known as cut-off points for
lactose intolerance affects 6–12% of Caucasians 1. Clinical history both SPT and specific IgE levels21 available in the
17
and up to 60–90% of other races . Lactose The clinical history is relevant in the diagnosis of literature. This indicates to clinicians whether a
intolerance is least common among Caucasians IgE-mediated FHS, non-IgE-mediated FHS and food challenge is needed, and the likelihood of
and most common among populations in the Far non-allergic FHS. Careful history taking and the outcome being positive.
East and Africa18 physical examination form the basis of diagnosis
.
of FHS and are explained in Table 1. Patch tests to food
Burden on the health system Table 1:The usefulness of a clinical history21 This test is used in the USA in the diagnosis of
allergic eosinophilic disease22,23 (see Glossary)
Allergic diseases across all ages costs the NHS an Taking a history can give useful information to the and in Europe for the diagnosis of atopic
19 22,23
estimated £900 million a year , mostly through health care professional regarding: dermatitis , but not generally in the UK.
prescribed treatments in primary care, represent- 1. Which diagnostic tests should be used, e.g. skin Although there are a few centres where this
ing 10% of the GP prescribing budget. The Health prick tests, blood tests or patch tests? diagnostic procedure is used, the usefulness of
Economy Data as presented by Professor Julian 2. Whether a food and symptom diary is needed the test is still debated and hence it is not widely
20 (although it is not always possible to identify the
Guest , lecturer in Pharmaceutical Medicine at used in the UK. The diagnosis and management
The University of Surrey, indicates that it costs the offending food(s) from these diaries alone) of eosinophilic disease and food protein enter-
NHS £23.6 million per year to manage cow’s milk 3. Which foods should be avoided during the opathies are usually dealt with in tertiary centres.
protein allergy in children. Treating one infant diagnostic test diet?
with an extensively hydrolysed formula for one 4. Whether a food challenge at home/hospital or 3. Diagnostic exclusion diets followed by a
year is estimated to cost £1,000. Using an amino gradual introduction of the food(s) may be required food challenge or food reintroduction
acid-based formula is estimated to cost £2,500. For many patients, particularly those suffering
2. Diagnostic tests from non-IgE-mediated allergy or non-allergic
Diagnosis of FHS Skin prick tests and specific IgE tests FHS, diagnosis can only be made by means of a
Both skin prick tests (SPT) and specific IgE tests combination of clinical history and dietary invest-
There are many routes to a diagnosis (or false are useful in the diagnosis of IgE-mediated food igations (diagnostic exclusion diets) followed by a
diagnosis) of food allergy and intolerance, such as allergy, but not for non-IgE-mediated food allergy food challenge or food reintroduction.
taking a clinical history, tests and food challenges, or non-allergic FHS. However, in most cases a Generally, all patients with either a history of
21
and food reintroduction . Figure 2 summarises health care professional cannot make a diagnosis immediate symptoms or positive SPT/specific IgE
the roles of different health care professionals in of food allergy based on SPT or blood test alone tests should be invited to a controlled setting, i.e.
under a doctor’s supervision and in the presence
of resuscitation equipment, for a food challenge21
.
Parents reporting symptoms of possible food allergy/intolerance A diagnostic diet could involve exclusion of a single
food such as cow’s milk, excluding a number of
foods such as cow’s milk, hen’s egg and wheat for
23
Health visitor/midwife/community nurse/community dietitian allergic eosinophilic disease , a few foods diet or a
Take history – may suggest preliminary avoidance of food(s) or specialised infant formula (see Table 2).
change the current formula Dietetic expertise is of particular importance
when dealing with infants’ and children’s diets and
progress should be monitored. Food exclusion
General practitioner diets are usually followed for a period of 2–3
May prescribe different formula in case of cow’s milk protein allergy weeks, but in diseases with fluctuating patterns
such as eczema it may be necessary to continue for
up to six weeks.
General practitioner with General paediatrician with Paediatric allergist
special interest in allergy special interest in allergy Prescribe different formula in Diagnosis of cow’s milk
May prescribe different formula Prescribe different formula in case of cow’s milk protein allergy hypersensitivity
in case of cow’s milk protein allergy case of cow’s milk protein allergy Obtain specific IgE test or SPTs
May obtain specific IgE test or May obtain specific IgE or may Make diagnosis An international task force has recently published
in very few cases may be able be able to perform SPT guidelines for the diagnosis and management of
to perform SPT May be able to make a diagnosis cow’s milk protein allergy (CMPA) in both breast-
May be able to make a diagnosis fed and formula-fed infants. These need to be
adjusted for local use taking into account the
May refer to dietitian for food health care system and health care provision in
Refer to dietitian for food Refer to specialist allergy each country24
avoidance and reintroduction avoidance followed by food . For a detailed discussion of this
dietitian for food avoidance 25
advice challenge or reintroduction followed by food challenge or topic, see Meyer .
Give advice regarding advice reintroduction advice Current guidelines for the UK are in progress,
maintenance diet and regular Give advice regarding Give advice regarding and are expected to include recommendations on
reassessment* maintenance diet and regular maintenance diet and regular the allergy care pathway including appropriate
reassessment* reassessment* usage of amino acid-based formula and extensively
hydolysed formula. Meanwhile, in the absence of
* In some cases emergency medication will need to be discussed with appropriate training by a nurse/allergy nurse/clinician. specific guidelines, the decision to use one of
Allergy nurses/paediatric nurses in some hospitals/centres may perform food challenges. these formulae for diagnostic purposes is a clinical
one and may differ between different centres,
Figure 2: The role of health care professionals in the diagnosis of food hypersensitivity depending on individual clinical preference.
129 © Journal of Family Health Care 2009 Vol 19 No 4 www.jfhc.co.uk
Learning files
Table 2: Different hydrolysed/amino acid-based formulae available in the UK
Formula Hypoallergenic characteristics Diagnostic use OTC Prescription
Partially hydrolysed formulae
Comfort 1 and Comfort 2 Partially hydrolysed whey Not recommended for diagnosis or management of cow’s milk protein Y N
(Cow & Gate) allergy/intolerance
Easy Digest (Aptamil) Partially hydrolysed whey Not recommended for diagnosis or management of cow’s milk protein
allergy/intolerance Y N
Extensively hydrolysed formulae
Pepti (Aptamil) Extensively hydrolysed whey To be used in diagnosis and management of CMPA in infants with N Y
Contains prebiotics IgE- or non-IgE-mediated allergy who first presented with symptoms
Contains almost 40% lactose and upon introduction of a cow’s milk formula without acute, severe
therefore more palatable reactions and/or growth faltering
– suitable for most children with
secondary lactose intolerance, but could
be a problem with primary lactose
intolerance as it is not lactose-free
Pepti Junior (Cow & Gate) Extensively hydrolysed whey To be used in diagnosis and management of CMPA in infants with
Clinically lactose-free IgE- or non-IgE-mediated allergy who first presented with symptoms
Contains 40% medium chain triglycerides upon introduction of a cow’s milk formula without acute, severe
reactions and/or growth faltering
Suitable for children with secondary lactose intolerance N Y
Nutramigen 1 and 2 Extensively hydrolysed casein To be used in diagnosis and management of CMPA in infants with IgE- Y Y
(Mead Johnson) Clinically lactose-free or non-IgE-mediated allergy who first presented with symptoms upon
introduction of a cow’s milk formula without acute, severe reactions
and/or growth faltering
Pregestimil (Mead Johnson) Extensively hydrolysed casein To be used in diagnosis and management of CMPA in infants with IgE- Y Y
Contains 54% medium chain triglycerides or non-IgE-mediated allergy who first presented with symptoms
(fat malabsorption) upon introduction of a cow’s milk formula without acute, severe
Clinically lactose-free reactions and/or growth faltering
Amino acid-based formula
Neocate (SHS) Elemental formula To be used in diagnosis and management of CMPA in infants with N Y
Neocate Advance and Neocate IgE-mediated-allergy: N Y
Active (over 1 year)
Nutramigen AA 1.Who reacted to cow’s milk protein in breast milk N Y
2.With history of acute, severe reactions Y N
3.With growth faltering
4.Whose symptoms continued on an extensively hydrolysed formula
5.With multiple food allergies
And in infants with non-IgE-mediated allergy:
1.Who reacted to cow’s milk protein in breast milk
2.With growth faltering
3.Whose symptoms continued on an extensively hydrolysed formula
or despite maternal avoidance of cow’s milk
4. Infants suffering with food protein enteropathy syndrome with
severe symptoms may also benefit from an amino acid formula (AAF)
5. Infants and children with multiple food allergies
6. Gut impairment conditions requiring an elemental diet, e.g.:
• Short bowel syndrome
• Maldigestion/malabsorption
• Intractable diarrhoea
• Inflammatory diseases of the bowel
Management of FHS Table 3: Dietary management of food Levels of avoidance
The input of a dietitian is paramount in the hypersensitivity Levels of avoidance required are currently based
management of food hypersensitivity (see Table 3 A dietary consultation will include: on:
for details of a typical dietary consultation). 1. Assessment of height, weight and dietary intake 1. The type of FHS from which the patient suffers.
2. Avoidance advice (Table 4), including understanding ● Most people with IgE-mediated food allergy
Avoidance food labels need to avoid the food completely,
3. Advice to ensure the diet is nutritionally adequate including trace amounts. However, some
A commonly presenting dilemma in clinical practice by providing information on substitute foods,“free people are able to tolerate cooked egg even
is whether to advise patients to strictly avoid the from”lists and special dietary products though they react to partially cooked egg
identified food or allow them to have small • Advice on practical aspects such as: cross- (e.g. in lightly cooked scrambled egg) or raw
contamination, eating in restaurants, going on egg (e.g. in mayonnaise)27
amounts on a regular basis when tolerated. Blanket holiday etc.When travelling abroad, translation . Some people are
advice of complete avoidance is difficult to follow, sheets and useful information can be obtained also able to tolerate heated milk products
has a huge impact on quality of life and may not be from www.allergyaction.co.uk or (e.g. in waffles and muffins) although they
essential for those children who tolerate small www.allergyuk.org or www.anaphylaxis.org.uk react to drinking pasteurised milk28
amounts. It could also lead to even more serious 4. Advice on suitable recipes, recipe books and ● Some people with non-IgE-mediated food
reactions in some children if accidental ingestion adaptation of family recipes allergy may be able to tolerate small
occurs26. Further evidence for the best approach of 5. Follow-up and reassessment to determine amounts of the food to which they are
managing this common problem is needed. development of tolerance allergic
www.jfhc.co.uk ©Journal of Family Health Care 2009 Vol 19 No 4 130
Learning files
Table 4: Checklist of foods and ingredients to avoid 90%) will tolerate the formula and improve when For all other types or presentations of cow’s milk
when suffering from food hypersensitivity to a using it. However, a small percentage (about 10%) protein allergies, an extensively hydrolysed
particular food. Source: may still be symptomatic and will therefore need formula can be used (see Figure 3 and Figure 4).
www.infantandtoddlerforum.org an amino acid-based formula.
Milk Extensively hydrolysed whey and extensively
Butter, Casein, Cheese, Cow/Sheep/Goat milk, Advice for breast-feeding mothers hydrolysed casein formulae
Evaporated or Condensed milk, Cream, Curd, Ghee, The first advice to the breast-feeding mother It is widely accepted that the palatability of extens-
Lactoglobulin, Lactose, Milk solids,Whey,Yoghurt should always be to try avoiding cow’s milk or ively hydrolysed whey (eHF-w) formulae (Aptamil
Egg foods containing cow’s milk in her own diet. If the Pepti) is superior to extensively hydrolysed casein
Albumin, Dried egg, Egg powder, Egg protein, Egg maternal elimination diet does not lead to any formulae (eHF-c)33 (Nutramigen). This is because
white and yolk, Frozen egg, Globulin, Lecithin (E322), improvement of symptoms despite very strong hydrolysation of the whey protein produces a more
Livetin, Ovalbumin, Ovoglobulin, Ovomucin, evidence of cow’s milk protein allergy in the infant, palatable product than hydrolysation of the casein
Ovovittellin, Pasteurised egg,Vitellin the only alternative may be to advise the mother to protein. (For more on palatability, see “Frequently
Wheat stop breast-feeding and to recommend the use of Asked Questions” Box on p.133.)
Bran, Cereal filler, Farina, Flour, Starch,Vegetable 30
protein,Wheat, Durum wheat, Semolina an amino acid-based formula . In addition, prebiotics have recently been added
Fish to the eHF-w (Aptamil Pepti), and two studies using
Choosing the most appropriate specialised this prebiotic mixture indicate an increase in
Anchovy (Worcestershire sauce),Aspic, Caviar infant formula probiotics (bifidobacteria and lactobacilli), reduced
Nuts (peanut or tree nuts) The choice of product depends on: growth of potentially harmful bacteria as well as a
Peanuts, Peanut oil which could also be called Arachis ● the age of the infant reduced allergic response and reduced recurrent
oil/Hypogeaia, Peanut flour, Peanut protein or any of ● the level of sensitivity to cow’s milk episodes of upper respiratory tract infection during
the tree nuts:Almond, Hazelnut,Walnut, Cashew, 34,35
Pecan nut, Brazil nut, Pistachio nut, Macadamia nut ● the presence of co-existing allergies the first year of life . These two industry-funded
and Queensland nut ● the immune mechanism involved studies, published in creditable peer-reviewed
Soya (IgE-mediated or non-IgE-mediated) journals, are accepted as convincing despite being
31 on small numbers of infants. Although the eHF-c
Hydrolysed vegetable protein, Soya lecithin, Soya ● the nutritional status of the infant
sauce, Miso, Soya albumin, Soya beans, Soya flour, Soya (see Table 1). may be less allergenic than the eHF-w, both these
milk, Soya nuts, Soya oil, Soya proteins, Soya sprouts, formulae have been used successfully in clinical
Tempeh,Texturised vegetable protein,Tofu Extensively hydrolysed formulae and amino acid- trials in infants suffering from: IgE-mediated cow’s
It is important that labels are checked every time a 36,37
product is bought as manufacturers may change the based formulae milk allergy (without a history of anaphylaxis) ,
As already mentioned, there are no clear guide- colic and/or inconsolable crying, and eczema38-40
recipes from time to time. (For more on advising lines in the UK regarding which formula (see (see Figure 3 and Figure 4).
patients how to interpret food labels, see "Frequently
Asked Questions" Box on p.133.) Glossary) to choose. It is, however, recom-
mended that an amino acid-based formula should Soya formulae
● Most people with non-allergic food be used when dealing with children with growth Soya formulae are not recommended for infants
hypersensitivity (lactose intolerance) will faltering32
, severe IgE-mediated cow’s milk allergy under six months of age, due the amount of iso-
be able to include small amounts of the (history of anaphylaxis or breathing difficulties), flavones that will be consumed per kg of body weight
food in their diet with no adverse effects severe eczema, or in children suffering from any in this age group and the risk of developing peanut
(see Table 4). 41
type of eosinophilic disease or food protein or soya allergy, though these risks may be small .
2. The characteristics of the particular food enteropathy. Soya formulae can therefore be used in infants not
protein and its degree of allergenicity, e.g. all allergic to soya after the age of six months, although
children with nut allergies need to avoid the Breast-fed infant with symptoms of cow’s soya is not considered to be the first choice of
food completely, whereas some people with milk protein allergy formula in many allergy centres. This is because
egg allergy may be able to tolerate small infants who are allergic to cow’s milk often react to
amounts of cooked egg soya as well41
Maternal avoidance of cow’s milk and . Despite these guidelines, the use of
3. The natural history of the particular FHS, e.g. 20
milk-containing foods – ensure adequate soya in the UK is still inappropriately high . Soya
most children will outgrow their milk allergy, but calcium intake formulae, e.g. Infasoy (Cow & Gate); Nurture Soya
only a few will outgrow their peanut allergy (see (Heinz); Isomil (Abbott); Prosobee (Mead Johnson);
“Frequently Asked Questions” Box on p.133). and Wysoy (SMA) may, however, be given to those
Symptoms resolve Symptoms do not infants who refuse extensively hydrolysed formulae.
Management of cow’s milk resolve
hypersensitivity Milk alternatives for children over two years of age
Continue with Amino acid-based For children over two years of age with a nutrit-
In addition to management of other FHS, man- avoidance and provide formula and provide ionally sound diet and sound nutritional status,
agement of cow’s milk protein allergy requires the follow-up follow-up cow’s milk alternatives include: soya milk; chufa
health care professional to choose the approp- milk derived from a succulent and trading under
riate formula (see Table 2, Figure 3 and Figure 4). the brand name of Tiger White; almond milk; oat
The European Society of Paediatric Gastro- Symptoms do not milk; coconut milk; quinoa drink (a milk derived
enterology, Hepatology and Nutrition (ESPGHAN) resolve from the quinoa plant); or potato milk. Rice milk
and the European Society of Pediatric Allergy and is no longer recommended for children under the
Clinical Immunology (ESPACI) stipulate that a age of four-and-a-half years because of concerns
hypoallergenic formula should be tolerated by Consider other food 42
allergy or other about the arsenic levels in these milks .
90% of infants with CMPA, with a 95% confidence medical cause
interval29
. This means that a formula can be Cautionary note: goat’s and ewe’s milk
considered as “hypoallergenic” if the vast majority Figure 3: Managing cow’s milk protein allergy in a breast-fed The use of goat’s milk and ewe’s milk in the
of children with cow’s milk protein allergy (about infant management of cow’s milk protein allergy is not
131 © Journal of Family Health Care 2009 Vol 19 No 4 www.jfhc.co.uk
no reviews yet
Please Login to review.