169x Filetype PDF File size 0.53 MB Source: elibrary.nefrosovet.ru
Nephrol Dial Transplant (2020) 35: 1–4
doi: 10.1093/ndt/gfz216
AdvanceAccess publication 7 November 2019
High-protein diet is bad for kidney health: unleashing the taboo
1 2 3 EDITORIAL
KamyarKalantar-Zadeh , Holly M. Kramer andDenisFouque
1 2
DivisionofNephrology,HypertensionandKidneyTransplantation,UniversityofCalifornia,Irvine,Orange,CA,USA, Departmentof
3 Downloaded from https://academic.oup.com/ndt/article-abstract/35/1/1/5614387 by guest on 18 February 2020
PreventiveMedicine,LoyolaUniversityChicago,Maywood,IL,USAand DepartmentofNephrology,CentreHospitalierLyonSud,
Lyon,France
Correspondence to: Kamyar Kalantar-Zadeh; E-mail: kkz@uci.edu; Twitter handle: @denisfouque1
Howoftenhaveyoubeentoldtoeatmoreproteinandlesscar- This trend has led to the ingestion of more meat and other
bohydratestostayhealthy?Thisisnotanemergingfoodculture animal-based foods, and the high-protein culture has emerged
but rather a prevailing dogma in our society. Physicians, dieti- as the preferred, healthy and safe way of eating at the dawn of
tians andotherhealthcareprofessionalstellusconstantlyabout the21stcentury.
the advantages of a high-protein diet (HPD), such as losing Is HPDsafeforkidneyhealthornot?Evidencesuggeststhat
weight rapidly, burning calories, diminishing appetite, prevent- theingestionofahigh-proteinmealleadstoincreasedglomeru-
ing obesity, managing metabolic syndrome and treating lar filtration rate (GFR), resulting in glomerular hyperfiltration
diabetes. This contemporary creed has gone so far that we feel as a result of the amino acid surge, which leads to dilatation of
continuously pressured to eat more protein and less carbohy- the afferent arteriole and increased intraglomerular pressure.
drates, including even less fruits and vegetables. We feel Inversely, a lower intake of dietary protein leads to more con-
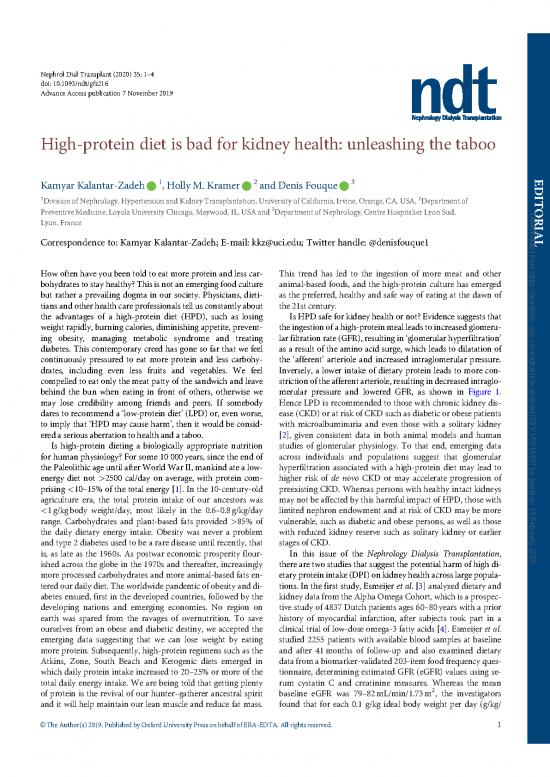
compelled to eat only the meat patty of the sandwich and leave striction of the afferent arteriole, resulting in decreased intraglo-
behind the bun when eating in front of others, otherwise we merular pressure and lowered GFR, as shown in Figure 1.
may lose credibility among friends and peers. If somebody Hence LPD is recommended to those with chronic kidney dis-
dares to recommend a low-protein diet (LPD) or, even worse, ease (CKD) or at risk of CKD such as diabetic or obese patients
to imply that HPD may cause harm, then it would be consid- with microalbuminuria and even those with a solitary kidney
eredaseriousaberrationtohealthandataboo. [2], given consistent data in both animal models and human
Is high-protein dieting a biologically appropriate nutrition studies of glomerular physiology. To that end, emerging data
for human physiology? For some 10 000years, since the end of across individuals and populations suggest that glomerular
the Paleolithic age until after World War II, mankind ate a low- hyperfiltration associated with a high-protein diet may lead to
energy diet not >2500 cal/day on average, with protein com- higher risk of de novo CKD or may accelerate progression of
prising <10–15% of the total energy [1]. In the 10-century-old preexisting CKD. Whereas persons with healthy intact kidneys
agriculture era, the total protein intake of our ancestors was maynotbeaffectedbythis harmful impact of HPD, those with
<1g/kgbody weight/day, most likely in the 0.6–0.8g/kg/day limited nephron endowment and at risk of CKD may be more
range. Carbohydrates and plant-based fats provided >85% of vulnerable, such as diabetic and obese persons, as well as those
the daily dietary energy intake. Obesity was never a problem with reduced kidney reserve such as solitary kidney or earlier
and type 2 diabetes used to be a rare disease until recently, that stages of CKD.
is, as late as the 1960s. As postwar economic prosperity flour- In this issue of the Nephrology Dialysis Transplantation,
ished across the globe in the 1970s and thereafter, increasingly there are two studies that suggest the potential harm of high di-
moreprocessed carbohydrates and more animal-based fats en- etary protein intake(DPI)onkidneyhealthacrosslargepopula-
tered our daily diet. The worldwide pandemic of obesity and di- tions. In the first study, Esmeijer et al.[3] analyzed dietary and
abetes ensued, first in the developed countries, followed by the kidneydatafromtheAlphaOmegaCohort,whichisaprospec-
developing nations and emerging economies. No region on tive study of 4837 Dutch patients ages 60–80years with a prior
earth was spared from the ravages of overnutrition. To save history of myocardial infarction, after subjects took part in a
ourselves from an obese and diabetic destiny, we accepted the clinical trial of low-dose omega-3 fatty acids [4]. Esmeijer et al.
emerging data suggesting that we can lose weight by eating studied 2255 patients with available blood samples at baseline
moreprotein. Subsequently, high-protein regimens such as the and after 41months of follow-up and also examined dietary
Atkins, Zone, South Beach and Ketogenic diets emerged in datafromabiomarker-validated203-itemfoodfrequencyques-
which daily protein intake increased to 20–25% or more of the tionnaire, determining estimated GFR (eGFR) values using se-
total daily energy intake. We are being told that getting plenty rum cystatin C and creatinine measures. Whereas the mean
2
of protein is the revival of our hunter–gatherer ancestral spirit baseline eGFR was 79–82mL/min/1.73m , the investigators
and it will help maintain our lean muscle and reduce fat mass. found that for each 0.1 g/kg ideal body weight per day (g/kg/
C
VTheAuthor(s)2019.PublishedbyOxfordUniversityPressonbehalfofERA-EDTA.Allrightsreserved. 1
Angiotensin
Low-protein pathway
diet modulators
Low-sodium
e
diet l
o
i
r
e
t
A r
f
f
e a
r
e
nt t
a n
r
t
e e
r r
i
o e
l
e f
f
E
Vasoconstriction Vasodilation
Intra-glomerular Downloaded from https://academic.oup.com/ndt/article-abstract/35/1/1/5614387 by guest on 18 February 2020
pressure
GFR
Mesangial (M)
cell signaling M M
TGF-β
Interstitial Tubule
fibrosis
FIGURE1:Theeffectsofalowproteinandlowsaltdiet on the afferent arteriole. (Adapted from Kalantar-Zadeh and Fouque [2].)
day) higher DPI, the annual GFR decline was accelerated by kidney function over time. Jhee et al. [5] took two additional
2
0.12mL/min/1.73m /year. The restricted cubic spline analy- steps to substantiate their findings. First, they divided the co-
ses showed a strictly linear association such that the lower the hort into those with and without kidney hyperfiltration and
DPI, the slower the rate of eGFR decline over time. Additional found that the faster drop in renal function happened only
analyses showed that patients with a daily total protein intake among those with preexisting hyperfiltration. Second, they
1.2g/kg/day had a 2-fold faster annual kidney function de- reexamined their analyses in another, even larger, cohort of
cline compared with <0.8g/kg/day, that is, a decline of 1.60 40 113 people from the Korean National Health and Nutrition
2
comparedwith0.84mL/min/1.73m ,respectively.Thesedata Examination Survey (2008–15) and found that the higher die-
did not find a superiority of plant- versus animal-based pro- tary protein quartile exhibited a higher risk of kidney hyperfil-
teins, which may be related to the fact that two-thirds of the av- tration. Of note, Jhee et al. [5] defined kidney hyperfiltration as
erage ingested protein was animal-based, making differential aneGFRwithadjustedresidualsgreaterthanthe95thpercentile
analyses less reliable. It is important to note that persons with and rapid renal function decline as a decline rate in eGFR
2
higher versus lower DPI >1.2 versus <0.8g/kg/day had a >3mL/min/1.73m /year. These definitions are population-
higher versus lower eGFR of 82618 versus 75619mL/min/ based arbitrary, and here again a regression to the mean can be
2
1.73m ,respectively[3]. This makes sense, given that higher apotentialreasonbehindthesefindings.Nevertheless,thebase-
proteinintakeincreasesGFRintheshortterm,whereasitaccel- line association of renal hyperfiltration with higher protein in-
erates kidneyfunctionlossinthelongterm,althoughregression take makes sense (see Figure 1)andthefasterdecreaseineGFR
tothemeanmaynotbefullyexcluded. inthelattergroupisbiologicallyplausible.
In the other study by Jhee et al. [5] in 9226 South Koreans There are other similar studies that have suggested the dele-
from a large national contemporary (2001–14) cohort, the terious effects of an HPD on kidney health [6]. A recent study
multivariate adjusted likelihood of kidney hyperfiltration was showed that among African Americans with diabetes, higher
3.5-fold higher in the highest versus lowest quartile of the DPI. protein intake as a percentage of total energy intake was associ-
As in the Dutch study by Esmeijer et al. [3], in the Korean ated with a greater decline in eGFR [7]. A large cohort study of
study, the loss of renal function was faster across higher quar- 1800healthy adults [8] showed that the highest versus lowest
tiles of DPI and the persons with the highest protein intake tertile of low-carbohydrate HPD was associated with a 48%
quartile exhibited 1.3-fold higher risk of a faster decline in greater risk of incident CKD. As to what types of protein are
2 K.Kalantar-Zadehetal.
Table 1. Recommended protein intake for different stages of kidney disease
Normalkidneyfunc- Mild to moderate AdvancedCKD Transitioning to dialy- Prevalent dialysis
a a a
tion (eGFR >60 ) and CKD(eGFR30–<60 ) (eGFR<30 )orany sis therapy with good therapy or any CKD
noproteinuria but at without substantial CKDwithsubstantial RKF,including incre- stage with existing or
d
higher CKDrisk, for proteinuria (<0.3g/ proteinuria mental dialysis imminent PEW
c c c
example, diabetes, day) (>0.3g/day) preparation
hypertension or
b
solitary kidney
Dietary protein <1.0g/kg/day, in- <1.0g/kg/day (con- 0.6–0.8g/kg/day 0.6–0.8g/kg/day on 1.2–1.4g/kg/day,
(g/kg/day crease proportion sider 0.6–0.8 if including 50% HBV nondialysis days mayrequire
based of plant-based eGFR<45mL/min or <0.6g/kg/day (e.g. incremental di- >1.5g/kg/day if
e with the addition of alysis) and >1.0g/ hypercatabolic
onIBW) proteins andfast
progression) EAA/KA kg/day on dialysis
days
Adapted from Kalantar-Zadeh and Fouque [2]. Downloaded from https://academic.oup.com/ndt/article-abstract/35/1/1/5614387 by guest on 18 February 2020
a 2
Theunit for eGFR is mL/min/1.73m body surface area.
b
Solitary kidney can be congenital, acquired or surgical, including status after donor or cancer nephrectomy.
c
Prevalent renal transplant recipients are often in the two categories of eGFR 30–<60mL/min and >30mL/min or transitioning to dialysis and can be approached similarly.
d
PEWaccordingtotheInternational Society of Renal Nutrition and Metabolism criteria [16].
e 2
The IBW is to be used for kilograms in the denominator of all dietary recommendations, especially in persons with a body mass index>30kg/m . IBW can be estimated in kilograms
in males (¼50kgþ2.3kg for each inch >5feet) and females (¼45.5kgþ2.3kg for each inch >5feet).
RKF, residual kidney function; HBV, high biologic value protein; EAA, essential amino acids; KA, ketoacids (keto-analogues of amino acids).
safer for kidneys, that is, plant- versus animal-based proteins, Metzger et al. [14] showed that the lower the DPI, even lower
there have been ongoing debates [9]. A recent study suggested than0.6g/kg/day, theslowertheprogressiontowardend-stage
that red and processed meats are associated with higher CKD renal disease, implying that there may be no clear sweat spot
risk, while nuts, low-fat dairy products and legumes appear to in the recommended range of low protein intake. However, it
be protective against the development of CKD [10]. There are is important to note that in CKD patients, PEW, which is often
studies suggesting that lower intake of meat- and animal-based heralded by a loss of appetite and unintentional reduction in
foods may be more beneficial to kidney and cardiovascular food ingestion, including lowered protein intake, may be asso-
health, given that the intake of animal fat is associated with al- ciated with worse CKD outcome, including faster CKD pro-
buminuria and given that other components related to meats, gression, as shown in a recent South Korean study [15]. This
suchascholineandcarnitine,areconvertedbygutfloraintotri- observational association is different from the causal impact of
methylamine (TMA) and TMA N-oxide, which are associated a proactively implemented LPD regimen on CKD progression.
withatherosclerosis and renal fibrosis [11]. Hence, during a PEW episode, an LPD for CKD management
As to whether an LPD with mostly to entirely plant-based shouldbetemporarilyhalted(Table1).
protein is adequate [12], it is important to note that the ThestudiesbyJheeetal.[5]andEsmeijeretal.[3]shouldbe
Recommended Dietary Allowance (RDA) for protein is 0.8g/ qualified for their epidemiologic nature, given that the associa-
kg/dayandthattheestimatedrequirementislikelyevenlower, tion does not equate to causality. The use of a food frequency
that is, 0.6g/kg/day, based on metabolic studies, provided ade- questionnaire in both studies is another limitation, since these
quate essential amino acids are ensured [2], whereas tradition- questionnaires tend to underestimate the average daily nutrient
ally an LPD for CKD management is defined as daily protein intake, although ranking subjects across their food intake such
in the 0.6–0.8g/kg/day range [2]. However, most adults in as in the form of quartiles of dietary protein is an effective
Western societies eat 1.0–1.4g/kg/day of protein [13]. remedy for the said shortcoming. Furthermore, glomerular
Whereas most guidelines recommend that 10–15% of energy hyperfiltration cannot be reliably detected by eGFR values.
be derived from protein, which is consistent with the RDA of Notwithstanding these limitations, these studies suggest that a
0.8g/kg/day of DPI, higher intakes of dietary protein, where high DPI may have deleterious effects on kidney health in the
protein intake may be as high as 20–25% or more of the general population, especially those with preexisting hyperfiltra-
total energy source, should not be prescribed to CKD patients tion or with other risk factors, such as a prior history of cardiovas-
or persons at high risk of CKD unless there are exceptional cular disease as was the case for the Alpha Omega study [3].
circumstances that would necessitate the intake of high Given these and other data, it is time to unleash the taboo and
amountsofproteinforlimitedperiodsoftime,suchastempo- make it loud and clear that a high-protein diet is not as safe as
rary corrective management for protein–energy wasting claimed, as it may compromise kidney health and result in a
(PEW) [2]. The recommended DPI for different stages of more rapid kidney function decline in individuals or populations
CKDare shown in Table 1 [2]. The target protein intake for at high risk of CKD. While more studies are needed to shed
CKDStages 3B, 4 and 5 as well as those with substantial pro- greater light, and while we expectthatdiscussionwillcontinue
teinuria is recommended to be 0.6–0.8g/kg/day, whereas for 17], it is prudent to avoid recom-
on this and other taboo topics [
persons without CKD but with a solitary kidney or at high mending high-protein intake for weight loss in obese or diabetic
risk of CKD, high protein intake >1.0g/kg/day should be patients or those with prior cardiovascular events or a solitary kid-
avoided. Indeed, a recent prospective observational study by neyif kidney health cannot be adequately protected.
Editorial 3
CONFLICTOFINTERESTSTATEMENT 7. Malhotra R, Lipworth L, Cavanaugh KL et al. Protein intake and long-term
Nonedeclaredrelevanttothisarticle. change in glomerular filtration rate in the Jackson heart study. JRenNutr
2018;28:245–250
(See related articles by Jhee et al. High-protein diet with renal 8. FarhadnejadH,AsghariG,EmamatHetal.Low-carbohydratehigh-protein
diet is associated with increased risk of incident chronic kidney diseases
hyperfiltration is associated with rapid decline rate of amongTehranianadults.JRenNutr2019;29:343–349
renal function: a community-based prospective cohort study. 9. Kalantar-Zadeh K, Moore LW. Does kidney longevity mean healthy vegan
Nephrol Dial Transplant 2020; 35: 98–106 and Esmeijer et al. foodandlessmeatorisanylow-proteindietgoodenough?JRenNutr2019;
Dietary protein intake and kidney function decline after myo- 29: 79–81
cardial infarction: the Alpha Omega Cohort. Nephrol Dial 10. Haring B, Selvin E, Liang M et al. Dietary protein sources and risk for inci-
dentchronickidneydisease:resultsfromtheatherosclerosisriskincommu-
Transplant2020;35:106–115) nities (ARIC) study. JRenNutr2017;27:233–242
11. Pignanelli M, Bogiatzi C, Gloor G et al. Moderate renal impairment and
toxic metabolites produced by the intestinal microbiome: dietary implica-
REFERENCES tions. J Ren Nutr 2019; 29: 55–64
1. World Health Organization. Chapter 3. Global and regional food 12. Joshi S, Shah S, Kalantar-Zadeh K. Adequacy of plant-based proteins in Downloaded from https://academic.oup.com/ndt/article-abstract/35/1/1/5614387 by guest on 18 February 2020
consumption patterns and trends. In Joint WHO/FAO Expert Consultation chronickidneydisease.JRenNutr2019;29:112–117
on Diet, Nutrition and the Prevention of Chronic Diseases. Geneva: World 13. MooreLW,Byham-GrayLD,ScottParrottJetal.Themeandietaryprotein
Health Organization, 2002. http://www.fao.org/3/ac911e/ac911e05.htm (10 intake at different stages of chronic kidney disease is higher than current
EDITORIAL October2019,datelastaccessed) guidelines. KidneyInt2013; 83:724–732
2. Kalantar-Zadeh K, Fouque D. Nutritional management of chronic kidney 14. Metzger M, Yuan WL, Haymann JP et al. Association of a low-protein diet
disease. NEnglJMed2017;377:1765–1776 withslowerprogressionofCKD.KidneyIntRep2018;3:105–114
3. Esmeijer K, Geleijnse JM, de Fijter JW et al. Dietary protein intake and kid- 15. Lee SW, Kim YS, Kim YH et al. Dietary protein intake, protein energy wast-
ney function decline after myocardial infarction: the Alpha Omega Cohort. ing, and the progression of chronic kidney disease: analysis from the KNOW-
NephrolDialTransplant2020;35:106–115 CKDstudy.Nutrients2019;11. pii: E121. doi: 10.3390/nu11010121
4. KromhoutD,GiltayEJ,GeleijnseJMetal.n-3fattyacidsandcardiovascular 16. FouqueD,Kalantar-ZadehK,KoppleJetal.Aproposednomenclatureand
events after myocardial infarction. N Engl J Med 2010; 363: 2015–2026 diagnostic criteria for protein-energy wasting in acute and chronic kidney
5. Jhee JH, Kee YK, Park S et al. High-protein diet with renal hyperfiltration disease. Kidney Int 2008; 73: 391–398
is associated with rapid decline rate of renal function: community-based 17. Moore LW, Kalantar-Zadeh K. Opportunities for renal nutrition and me-
prospective cohortstudy. Nephrol Dial Transplant2020; 35: 98–106 tabolism at the dawn of 2020s: an inauguration message from the new
6. KoGJ, ObiY,TortoriciAR etal. Dietary protein intake and chronic kidney JRENeditors-in-chief. JRenNutr2019; 29: 1
disease. Curr Opin Clin Nutr Metab Care 2017; 20: 77–85 Received: 26.5.2019; Editorial decision: 17.9.2019
Nephrol Dial Transplant (2020) 35: 4–9
doi: 10.1093/ndt/gfz219
2019 Update in basic kidney research: microbiota in chronic
kidney disease, controlling autoimmunity, kidney inflammation
andmodelling the glomerular filtration barrier
Hans-JoachimAnders
RenalDivision,DepartmentofMedicineIV,UniversityHospital,LMUMunich,Mu¨nchen,Germany
Correspondence to: Hans-Joachim Anders; E-mail: hjanders@med.uni-muenchen.de; Twitter handle: @hjanders_hans
Recently, NDTpublishedaseriesofexcitingarticlesinthebasic a robust polyclonal immune complex glomerulonephritis mim-
kidneyresearchdomain. ickingmanymorphologicalaspectsofprogressivelupusnephri-
In the April issue, the team of Lingyun Sun reported their tis in humans. The authors isolated MSC from human
6
studies on the therapeutic effects of human umbilical cord- umbilical cords and transplanted 110 cells into 6-month-
derived mesenchymal stromal cells (UC-MSC) in MRL-Faslpr old female MRL-Faslpr mice as a single tail vein injection. A
mice[1].Noneoftheavailablerodentmodelsusedtostudysys- similar numberofhumanembryoniclungfibroblastsorvehicle
temic lupus erythematosus adequately mimics human lupus, was injected into mice of two control groups, respectively. All
butMRL-Faslprmicearefrequentlyusedtostudylupusnephri- mice were sacrificed 2months later. Mice transplanted with
tis because they develop lupus-like systemic autoimmunity with UC-MSC had lower circulating double-stranded DNA
C
VTheAuthor(s)2020.PublishedbyOxfordUniversityPressonbehalfofERA-EDTA.Allrightsreserved. 4
no reviews yet
Please Login to review.