203x Filetype PDF File size 0.29 MB Source: academic.oup.com
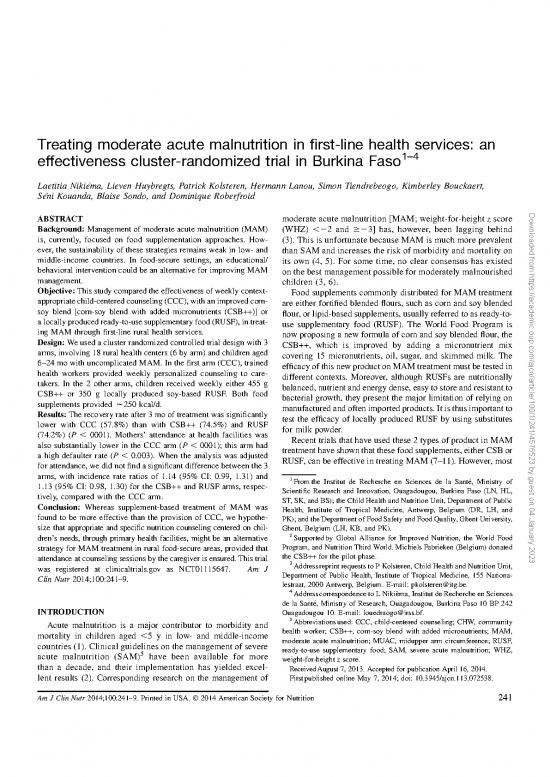
Treating moderate acute malnutrition in first-line health services: an
effectiveness cluster-randomized trial in Burkina Faso1–4
`
Laetitia Nikiema, Lieven Huybregts, Patrick Kolsteren, Hermann Lanou, Simon Tiendrebeogo, Kimberley Bouckaert,
´
Seni Kouanda, Blaise Sondo, and Dominique Roberfroid
ABSTRACT moderate acute malnutrition [MAM; weight-for-height z score Downloaded from https://academic.oup.com/ajcn/article/100/1/241/4576523 by guest on 04 January 2023
Background: Management of moderate acute malnutrition (MAM) (WHZ) ,22and$23] has, however, been lagging behind
is, currently, focused on food supplementation approaches. How- (3). This is unfortunate because MAM is much more prevalent
ever, the sustainability of these strategies remains weak in low- and than SAMandincreasestheriskofmorbidityandmortalityon
middle-income countries. In food-secure settings, an educational/ its own (4, 5). For some time, no clear consensus has existed
behavioral intervention could be an alternative for improving MAM onthebestmanagementpossibleformoderatelymalnourished
management. children (3, 6).
Objective: This study compared the effectiveness of weekly context- Food supplements commonly distributed for MAM treatment
appropriate child-centered counseling (CCC), with an improved corn- are either fortified blended flours, such as corn and soy blended
soy blend [corn-soy blend with added micronutrients (CSB++)] or flour, or lipid-based supplements, usually referred to as ready-to-
a locally produced ready-to-use supplementary food (RUSF), in treat- use supplementary food (RUSF). The World Food Program is
ing MAM through first-line rural health services. nowproposing a new formula of corn and soy blended flour, the
Design: We used a cluster randomized controlled trial design with 3 CSB++, which is improved by adding a micronutrient mix
arms, involving 18 rural health centers (6 by arm) and children aged covering 15 micronutrients, oil, sugar, and skimmed milk. The
6–24 mo with uncomplicated MAM. In the first arm (CCC), trained efficacyofthisnewproductonMAMtreatmentmustbetestedin
health workers provided weekly personalized counseling to care- different contexts. Moreover, although RUSFs are nutritionally
takers. In the 2 other arms, children received weekly either 455 g balanced, nutrient and energy dense, easy to store and resistant to
CSB++ or 350 g locally produced soy-based RUSF. Both food bacterial growth, they present the major limitation of relying on
supplements provided w250 kcal/d. manufacturedandoftenimportedproducts.Itisthusimportantto
Results: The recovery rate after 3 mo of treatment was significantly test the efficacy of locally produced RUSF by using substitutes
lower with CCC (57.8%) than with CSB++ (74.5%) and RUSF for milk powder.
(74.2%) (P , 0001). Mothers’ attendance at health facilities was Recent trials that have used these 2 types of product in MAM
also substantially lower in the CCC arm (P , 0001); this arm had treatment have shown that these food supplements, either CSB or
a high defaulter rate (P , 0.003). When the analysis was adjusted RUSF, can be effective in treating MAM (7–11). However, most
for attendance, we did not find a significant difference between the 3
arms, with incidence rate ratios of 1.14 (95% CI: 0.99, 1.31) and 1 ´
1.13 (95% CI: 0.98, 1.30) for the CSB++ and RUSF arms, respec- Fromthe Institut de Recherche en Sciences de la Sante, Ministry of
tively, compared with the CCC arm. Scientific Research and Innovation, Ouagadougou, Burkina Faso (LN, HL,
ST, SK, and BS); the Child Health and Nutrition Unit, Department of Public
Conclusion: Whereas supplement-based treatment of MAM was Health, Institute of Tropical Medicine, Antwerp, Belgium (DR, LH, and
found to be more effective than the provision of CCC, we hypothe- PK);andtheDepartmentofFoodSafetyandFoodQuality,GhentUniversity,
size that appropriate and specific nutrition counseling centered on chil- Ghent, Belgium (LH, KB, and PK).
dren’s needs, through primary health facilities, might be an alternative 2Supportedby Global Alliance for Improved Nutrition, the World Food
strategy for MAM treatment in rural food-secure areas, provided that Program, and Nutrition Third World. Michiels Fabrieken (Belgium) donated
attendance at counseling sessions by the caregiver is ensured. This trial the CSB++ for the pilot phase.
3Addressreprint requests to P Kolsteren, Child Health and Nutrition Unit,
was registered at clinicaltrials.gov as NCT01115647. Am J
Clin Nutr 2014;100:241–9. Department of Public Health, Institute of Tropical Medicine, 155 Nationa-
lestraat, 2000 Antwerp, Belgium. E-mail: pkolsteren@itg.be.
4 `
Addresscorrespondence to L Nikiema, Institut de Recherche en Sciences
´
de la Sante, Ministry of Research, Ouagadougou, Burkina Faso 10 BP 242
INTRODUCTION Ouagadougou 10. E-mail: louedraogo@irss.bf.
5Abbreviationsused: CCC, child-centered counseling; CHW, community
Acute malnutrition is a major contributor to morbidity and
mortality in children aged ,5 y in low- and middle-income health worker; CSB++, corn-soy blend with added micronutrients; MAM,
countries (1). Clinical guidelines on the management of severe moderate acute malnutrition; MUAC, midupper arm circumference; RUSF,
5 ready-to-use supplementary food; SAM, severe acute malnutrition; WHZ,
acute malnutrition (SAM) have been available for more weight-for-height z score.
than a decade, and their implementation has yielded excel- ReceivedAugust 7, 2013. Accepted for publication April 16, 2014.
lent results (2). Corresponding research on the management of Firstpublished online May 7, 2014; doi: 10.3945/ajcn.113.072538.
AmJClin Nutr 2014;100:241–9. Printed in USA. 2014 American Society for Nutrition 241
`
242 NIKIEMA ETAL
of these trials used industrialized products in quantities repre- Children aged 6–24 mo, with uncomplicated MAM (WHZ
senting the daily recommended intake of calories. Moreover, the ,22and$23basedonthe2006WHOgrowthreference)(23)
downside of food supplementation is that it does not really ad- and living in the catchment area of a health center were cu-
dress the causes of malnutrition and assumes that malnutrition mulatively included in the trial until the preset sample size was
equals a lack of food at the household level. Factors such as the fulfilled. MAM children were either detected passively via the
cost of supplements and the need for external donor support can routine growth-monitoring program or at consultations for sick
affect sustainability and scaling up. Furthermore, there is a risk children, or actively through a monthly community-based
of overlooking careful diagnosis of the causes of MAM by screening. Children with a diagnosis of SAM (presence of pit-
simplifying MAM management to general food supplementa- ting edema or WHZ ,23, without complications) were ex-
tion interventions. Offering cause-related counseling holds great cluded from the trial and treated according to the national
potential but its evidence base is surprisingly scant. A patient- protocol for SAM. Child age was either determined on the basis
centered counseling approach is increasingly considered crucial of an official document such as a health card or a birth certificate
for the delivery, of high-quality health care (12–14). These ed- when available or by approximation with the help of a locally
ucational and behavioral interventions can be effective at im- adapted events calendar. Downloaded from https://academic.oup.com/ajcn/article/100/1/241/4576523 by guest on 04 January 2023
proving child growth (15–17). However, evidence of their efficacy Informed consent was obtained from all participating care-
in treating MAM is lacking (18, 19). takers before inclusion. All children received the preventive
In this study we aimed to compare the effectiveness of a child- treatments (vaccination, vitamin A supplementation, and deworming)
centered counseling (CCC) compared with the provision of either recommended by the Ministry of Health according to their age at
CSB++ or a locally produced RUSF with soy flour that substitutes the time of inclusion. All children were examined weekly, and all
milkpowder,inprimaryhealthcareservicesfortreatingMAMcases. medical treatments provided during the study were given for free.
Theproposal was approved by the research ethical committee of
Burkina Faso and the ethical committee of Antwerp University,
SUBJECTS AND METHODS Belgium.
Study design
This cluster-randomized controlled trial was carried out in the Intervention
´ Health workers in the CCC arm were trained in communi-
health district of Hounde, located in the Western region of
Burkina Faso, with 27 functional primary health services. This cation and nutrition counseling by using a child-centered ap-
setting was selected for 2 reasons. First, the food insecurity was proach based on the model developed by Stewart et al (24). This
quite low (20), which allowed considering an approach of model took into account 6 interconnecting components: 1) ex-
counseling only. The district had a high cereal production and ploring both disease and illness experience, 2) understanding the
one of the lowest prevalence of wasting in children ,5 y of age whole person, 3) finding common ground regarding manage-
reported in the country in 2012 (11.1% compared with the na- ment, 4) incorporating prevention and health promotion, 5) en-
tional estimate of 15.5%) (21). Prevalence of MAM was 7.8% in hancing the doctor patient relation, and 6) being realistic about
´ personal limitations and issues such as the availability of time
Hounde district in the same period. Moreover, as in the rest of
the country, MAM treatment recommendations provided to the and resources.
caretakers were quite general, and mothers received nonspecific The training comprised 2 phases. The first one involved
dietary advice through health services or community channels, a formal training based on the Manual on Counseling the Mother
underlying the need for another counseling approach. Second, from the Integrated Management of Child Illness Guidelines
a production unit of lipid-based nutrient supplements was al- (25) and on specific communication techniques on all aspects of
ready put into place in an earlier intervention study (22). the patient-centered approach. Dietary recommendations were
Aclusterwasdefinedbyahealthcenteranditscatchmentarea. based on the PAHO/WHO Guiding Principles for Complemen-
Eighteenruralhealthcenters(clusters)wereshort-listedbasedon tary Feeding of the Breastfed Child (26) and the WHO Guiding
high prevalence of MAM, size of covered population, and agree- Principles for Feeding Non-Breastfed Children 6–24 Months of
ment of health workers to participate in the study, as assessed in Age (27). The second phase was carried out over 3 d and in-
a preliminary survey. These health centers were randomly allo- volved practical training that featured role-play and case studies.
cated to 1 of the 3 arms of the study: CCC, CSB++, or RUSF, with A refresher training was organized at months 6 and 12 of the
6 clusters in each arm. intervention. Formative supervision sessions were carried out
Random allocation was performed in public by the heads of quarterly by the district nutrition officers to address identified
eachhealthcenterwhowereinvitedtodraw1paperfromabasket weaknesses in service delivery and questions raised by health
containing 18 pieces of paper (6 papers for each of the study workers.
arms). This was done under the supervision of the principal During the first visit of the child, trained health workers
investigator during the launch meeting. recorded the child’s medical history, feeding, care practices, and
The sample size was calculated by using PASS software characteristics of the family (family size, socioeconomic char-
(HintzeJ.PASS2008NCSSLLC;www.ncss.com)andwassetat acteristics, and hygiene practice). This information was then used
116participants per cluster, or 696 per arm with an a-error = 5%, to identify, together with the caretaker, the most important causes
a b-error = 20%, an expected recovery rate in any group of 70%, of the child’s poor health. A case-specific treatment strategy was
an expected difference in recovery rate among groups consid- then developed and implemented. During subsequent weekly
ered of public health importance of 10% points, and an intra- consultations, health workers assessed how the strategy was im-
class correlation of 0.01. plemented, identified promoting or blocking factors, and adapted
CHILD-CENTERED COUNSELING IN MAM MANAGEMENT 243
the treatment plan further in agreement with the caretakers. All from the Department of Food Safety and Food Quality at Ghent
corresponding observations and discussions were reported in the University (LH).
child’s individual file. A counseling session took approximately Both food supplements, CSB++ and RUSF, provided similar
1.5 h the first time and 45 min during follow-up visits. quantitiesofenergy(250kcal/d).Theywereintendedasabooster
After eachweeklyconsultation,caretakerswerealsoinvitedto facilitating accelerated growth in a food secure population of
cooking sessions where recipes for optimizing child meals with breastfed children. In both dietary supplement arms, it was duly
local ingredients were shared. Each child had an individual file in emphasized to caretakers that food supplements were intended
which all medical information, advice received, issues with only for children with MAM. In the CSB++ and RUSF groups,
implementation of the strategy, and identified alternatives to the parents received the usual generic nutrition advice given by
strategy were recorded. health services, such as to continue breastfeeding, to increase
In the second arm of the study, children received daily 65 g dietary diversity, and to frequently provide nutrient-dense snacks.
CSB++. Mothers were advised to dilute this amount in 370 g All children, regardless of group allocation, received vitamin
water (roughly equivalent to 5 measures of a traditional flour A (100,000 IU for children 6–12 mo of age, 200,000 IU for
ladle) and cook it until simmering for 5 to 10 min. CSB++ was children .1 y of age) and 100 mg mebendazole (1 tablet 2 Downloaded from https://academic.oup.com/ajcn/article/100/1/241/4576523 by guest on 04 January 2023
preparedfromheat-treatedmaize(57–62%),dehulledsoyabeans times/d for 3 d). Those with anemia (hemoglobin ,11 g/dL)
(15–20%), sugar (9%), dried skim milk (8%), refined soybean oil weregiven iron + folic acid syrup (100 mg; 1 dose 3 times/d) for
(3%), vitamins and minerals (0.20%), calcium carbonate (1.19%), 4 wk. Vaccinations were also administered according to the
monocalcium phosphate (0.80%), and potassium chloride (0.76%) national schedule.
(Table 1). The CSB++ was provided by World Food Program and Weekly follow-up visits were scheduled for up to 3 mo after
distributed to children with MAM weekly. inclusion. Children missing a weekly visit in the health center
In the third study arm, children received daily 50 g (3 ta- were home-visited to encourage parents to continue their par-
blespoons) of a fortified spread (8), in which milk powder was ticipation in the study. In the CSB++ and RUSF arms the home
replaced by soy flour to reduce cost. This locally produced RUSF visits were carried out by community health workers (CHWs),
was composed of peanut butter (26%), vegetable oil (12.5%), who also brought along the food supplements. In the CCC arm,
sugar (25%), whole soy flour (33%), shea butter (2.0%), and the homevisits were conducted by the nurses of the health center
multiple micronutrients (1.5%). The micronutrient powder was so as to deliver CCC. In case of refusal to continue participation,
obtained from Nutriset. The nutritional composition of a daily monitoring of the child was stopped. If a child missed 4 con-
dose of RUSF is shown in Table 1. The local RUSF quality and secutive follow-up visits despite home visits by CHWs or nurses,
safety assessment was carried out by a food science engineer heorshewasdeclaredadefaulter,butwasnotexcludedfromthe
trial. The definition of defaulter was relaxed from what was
TABLE1 planned in the protocol (missing 2 consecutives visits), because,
1
Nutrient content of the daily ration of CSB++ and RUSF during the pilot phase in the rainy season, there were many cases
CSB++ per 65 g RUSF per 50 g of involuntary absence (inaccessibility of areas, or unavailability
of parents) in up to 2 consecutive visits, with a return of the
Energy (kcal) 273.0 258.3 child later in the trial. Reasons for defaulting were investigated
Protein (g) 10.4 8.7 by interviewing a subsample of 45 mothers and 19 fathers.
Fat (g) 5.9 17.4 Loss to follow-up was defined as no information for children
Calcium (mg) 390.0 322.4
Phosphorus (mg) 130.0 282.7 at the end of the trial. Recovery was defined as a WHZ $22.
Potassium (mg) 260.0 NR The definition of this outcome, initially set at WHZ $21, also
2 changed after the trial pilot phase. Indeed, it required more time
Magnesium (mg) NR 21.1
Iron (mg) 4.2 11.1 for a child to reach WHZ $21 and increased the cost of the
Zinc (mg) 3.3 10.2 intervention, whereas the cutoff of WHZ $22 is internationally
2
Copper (mg) NR 0.2 acknowledged. Failure to recover was defined by a WHZ ,22
2
Selenium (mg) NR 17.8 after 3 mo of treatment. Failed children underwent a complete
2
Manganese (mg) NR 0.2 clinical check-up to diagnose underlying pathologies and were
2
Iodine (mg) 26.0 94.8
Vitamin A (mg) NR 480.2 followed-up until recovery. Weight, length, and midupper arm
Thiamin (mg) 0.1 1.2 circumference (MUAC) were measured on enrollment and at
Riboflavin 0.3 NR each follow-up visit. Weight was measured by using UNI-
Niacin (mg) 3.1 9.0 SCALEelectronic scales with an accuracy within 100 g (SECA
2
Pantothenic acid (mg) 4.4 2.6 Germany). Length was measured with a rigid length board to the
Vitamin B-6 (mg) 1.1 0.7 nearest millimeter (Short Productions), and MUAC was mea-
Vitamin B-12 (mg) 1.3 1.1 sured with a nonstretchable tape with an accuracy of 1 mm
Folic acid (mg) 39.0 225.8 (model 201; SECA Germany). All measurements were done in
Vitamin C (mg) 65.0 81.2
Vitamin D (mg) 2.6 NR duplicate, and the mean of the measurements was used for
2 analysis. Information on child age, feeding practices, household
Vitamin E (mg) 5.4 8.1
Vitamin K (mg) 65.0 NR composition, socioeconomic status, child morbidity within the
1CSB++, corn-soy blend with added micronutrients; NR, not reported; 2wkprecedingthevisit, and the medical history of the child and
RUSF, ready-to-use supplementary food. mother were also recorded at enrollment. A socioeconomic in-
2Novalues for food matrix (only CMV, a mix of vitamins and minerals dexwasderived by using principal component analysis based on
in powder). the possession of animals, housing, furniture, and housing
`
244 NIKIEMA ETAL
characteristics (28). Attendance was calculated as the proportion counseling session attendance to receive the intervention in the
of the actual number of follow-up visits over the number of CCCarm,andthenonrandomdistribution of defaulter cases, we
visits expected between inclusion and exit dates. Adherent in- also conducted some exploratory analysis. First, we repeated the
dividuals were defined as individuals with an attendance $80%. analysis on the subgroup of nondefaulters. Second, we adjusted
the intent-to-treat analyses as recommended (29, 30) by using
Data analysis attendance (in tertiles) as an instrumental variable. Statistical
significance was set at 5% for all tests. All statistical analyses
Duplicate data entry into EpiData version 3.1 (EpiData As- were conducted by using Stata 12.0 (StataCorp).
sociation)andavaliditycross-checkwereperformed.Descriptive
statistics were used to describe the sample and to compare
children at baseline between arms. RESULTS
Comparisons between arms of the primary outcomes (de- Between12July2010and17November2011,1974episodesof
faulter, recovery, SAM, MAM, and death), attendance, time to uncomplicatedMAMwereincludedin1ofthe3trialarms(Figure
recovery, weight, length, and daily MUAC gains were made by 1), corresponding to 1824 unique children. A total of 144 children Downloaded from https://academic.oup.com/ajcn/article/100/1/241/4576523 by guest on 04 January 2023
using linear mixed-effects models for continuous outcomes,
whereas mixed-effects logistic regression models were used for were included twice and 6 children 3 times, with no significant
proportions, with health center and individual as random effects. difference between the arms: 38 (6.3%), 55 (8.1%), and 57 (8.2%),
Individual outcomes underwent an intent-to-treat analysis. The respectively, in the CCC, CSB++, and RUSF arms. No difference
proportional hazard assumption was visually appraised by in- in baseline characteristics were found between children included
specting the Kaplan-Meier plots. Censoring for death, default, once and those who were re-enrolled (data not shown).
SAM or treatment failure was done at the time of the last in- Baseline characteristics of all enrolled children appeared
dividual clinic visit. A log-rank test was used to compare trends balanced amongthe3trialarms,exceptthatthenutritionalstatus
over time between the 3 survival curves. of mothers (BMI) and children (as measured by MUAC and
Differencesinchildrecoverybetweentrialarmsweretestedby height-for-age z score, but not WHZ) and child morbidity was
using a mixed-effects Poisson regression model, with health slightly better in the RUSF arm (Table 2). The mean (6SD) age
center and child as random effects. The random effect at the at enrollment was 13.4 6 4.6 mo. Most of the mothers were
individual level accounted for cases of relapse with children illiterate (82.6%). More than 65% of children had suffered from
entering the trial at least twice. Concerning the importance of a morbid episode in the preceding 2 wk.
FIGURE1.Trialprofile.Losttofollow-upwasdefinedasnoinformationforchildrenattheendofthetrial.Mostofthechildrenhadleftthearea.Defaulter
was defined as an absence of information at 4 consecutive visits. Failure was defined as being still moderately malnourished (MAM; 23.00 # WHZ ,22
SD; WHO 2006 reference) at the end of the observation period. Recovery was defined as a WHZ $22 SD (WHO 2006 reference). CCC, child-centered
counseling; CSB++, corn soy blend with added micronutrients; MAM, moderate acute malnutrition; RUSF, ready-to-use supplementary food; SAM, severe
acute malnutrition (WHZ ,23.00 SD; WHO 2006 reference); WHZ, weight-for-height z score.
no reviews yet
Please Login to review.