236x Filetype PDF File size 0.75 MB Source: www.bsuh.nhs.uk
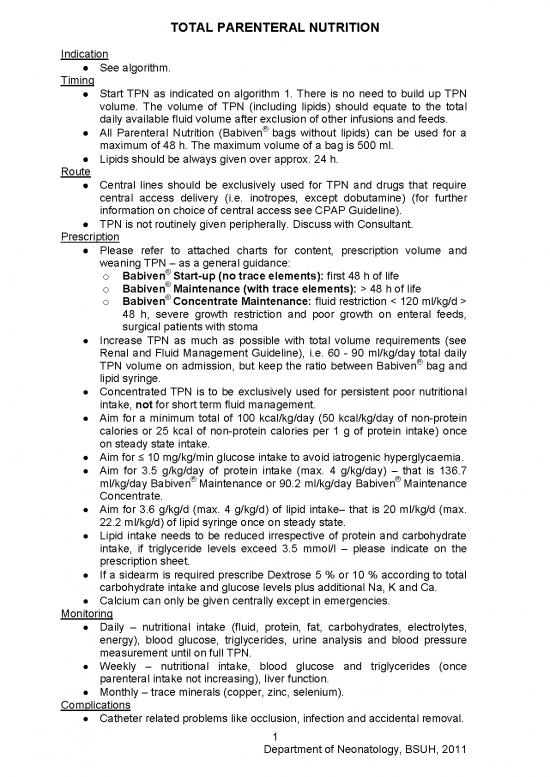
TOTAL PARENTERAL NUTRITION
Indication
See algorithm.
Timing
Start TPN as indicated on algorithm 1. There is no need to build up TPN
volume. The volume of TPN (including lipids) should equate to the total
daily available fluid volume after exclusion of other infusions and feeds.
All Parenteral Nutrition (Babiven® bags without lipids) can be used for a
maximum of 48 h. The maximum volume of a bag is 500 ml.
Lipids should be always given over approx. 24 h.
Route
Central lines should be exclusively used for TPN and drugs that require
central access delivery (i.e. inotropes, except dobutamine) (for further
information on choice of central access see CPAP Guideline).
TPN is not routinely given peripherally. Discuss with Consultant.
Prescription
Please refer to attached charts for content, prescription volume and
weaning TPN – as a general guidance:
o Babiven® Start-up (no trace elements): first 48 h of life
o Babiven® Maintenance (with trace elements): > 48 h of life
o Babiven® Concentrate Maintenance: fluid restriction < 120 ml/kg/d >
48 h, severe growth restriction and poor growth on enteral feeds,
surgical patients with stoma
Increase TPN as much as possible with total volume requirements (see
Renal and Fluid Management Guideline), i.e. 60 - 90 ml/kg/day total daily
®
TPN volume on admission, but keep the ratio between Babiven bag and
lipid syringe.
Concentrated TPN is to be exclusively used for persistent poor nutritional
intake, not for short term fluid management.
Aim for a minimum total of 100 kcal/kg/day (50 kcal/kg/day of non-protein
calories or 25 kcal of non-protein calories per 1 g of protein intake) once
on steady state intake.
Aim for ≤ 10 mg/kg/min glucose intake to avoid iatrogenic hyperglycaemia.
Aim for 3.5 g/kg/day of protein intake (max. 4 g/kg/day) – that is 136.7
ml/kg/day Babiven® Maintenance or 90.2 ml/kg/day Babiven® Maintenance
Concentrate.
Aim for 3.6 g/kg/d (max. 4 g/kg/d) of lipid intake– that is 20 ml/kg/d (max.
22.2 ml/kg/d) of lipid syringe once on steady state.
Lipid intake needs to be reduced irrespective of protein and carbohydrate
intake, if triglyceride levels exceed 3.5 mmol/l – please indicate on the
prescription sheet.
If a sidearm is required prescribe Dextrose 5 % or 10 % according to total
carbohydrate intake and glucose levels plus additional Na, K and Ca.
Calcium can only be given centrally except in emergencies.
Monitoring
Daily – nutritional intake (fluid, protein, fat, carbohydrates, electrolytes,
energy), blood glucose, triglycerides, urine analysis and blood pressure
measurement until on full TPN.
Weekly – nutritional intake, blood glucose and triglycerides (once
parenteral intake not increasing), liver function.
Monthly – trace minerals (copper, zinc, selenium).
Complications
Catheter related problems like occlusion, infection and accidental removal.
1
Department of Neonatology, BSUH, 2011
Compatibility related problems – check stability matrix in unit drug folder.
Parenteral nutrition related problems, e.g. hyperglycaemia, conjugated
hyperbilirubinaemia, acidosis.
Algorithm 1.
2
Department of Neonatology, BSUH, 2011
Composition of Available Formulas (Babiven®)
Composition Start-up Bag Maintenance Bag Maintenance Maintenance Bag
(with trace elements) Bag (Concentrate)
Volume per 100ml per 100ml per 100ml per 66ml
Nitrogen(g) 0.43 0.36 0.37 0.37
Amino acids(g) 3 2.53 2.56 2.56
Glucose (g) 10 11.0 11.11 11.1
Non protein kcal 40 43.96 44.44 44.4
Sodium (mmol) 0 2.2 2.22 2.2
Potassium (mmol) 1 1.49 1.5 1.5
Calcium (mmol) 1 1.1 1.11 1.11
Magnesium (mmol) 0.2 0.14 0.15 0.15
Phosphate (mmol) 1 1.1 1.11 1.11
Chloride (mmol) 0 1.47 1.5 1.5
Acetate (mmol) 0 1.49 1.5 1.5
Zinc (micromol) 4 3.79 0 0
Parenteral Nutrition Prescription Excluding Lipids
(Start-up Bag)
Volume of parenteral nutrition Non-protein calories Carbohydrates Protein
in ml/kg/day in kcal/kg in mg/kg/min in g/kg/day
10 4 0.7 0.3
20 8 1.4 0.6
30 12 2.1 0.9
40 16 2.8 1.2
50 20 3.5 1.5
60 24 4.2 1.8
70 28 4.8 2.1
80 32 5.5 2.4
90 36 6.2 2.7
100 40 6.9 3
110 44 7.7 3.3
120 48 8.4 3.6
130 52 9.1 3.9
140 56 9.8 4.2
Parenteral Lipid Infusion
Volume of lipid infusion Non-protein calories Lipids
in ml/kg/day in kcal/kg in g/kg/day
5 9.1 0.9
5.5 10.0 1.0
10 18.3 1.8
11 20.1 2
15 27.4 2.7
16.5 30.2 3
20 36.6 3.6
22 40.2 4
25 45.7 4.5
3
Department of Neonatology, BSUH, 2011
Parenteral Nutrition Prescription Excluding Lipids
(Maintenance Bag – No Trace Elements)
Volume of Non-protein calories Carbohydrates Protein Volume of
normal volume PN In kcal/kg in mg/kg/min in /kg/day concentrated PN
in ml/kg/day in ml/kg/day
10 4.4 0.8 0.3 6.6
20 8.9 1.5 0.5 13.2
30 13.3 2.3 0.8 19.8
40 17.8 3.1 1.0 26.4
50 22.2 3.9 1.3 33.0
60 26.7 4.6 1.6 39.6
70 31.1 5.4 1.8 46.2
80 35.6 6.2 2.1 52.8
90 40.0 6.9 2.3 59.4
100 44.4 7.7 2.6 66.0
110 48.9 8.5 2.8 72.6
120 53.3 9.3 3.1 79.2
130 57.8 10.0 3.4 85.8
136.7 60.7 10.5 3.5 90.2
140 62.2 10.8 3.6 92.4
150 66.7 11.6 3.9 99.0
156.3 69.5 12.1 4.0 103.2
Parenteral Nutrition Prescription Excluding Lipids
(Maintenance Bag with Trace Elements)
Volume of Non-protein calories Carbohydrates Protein Volume of
normal volume PN In kcal/kg in mg/kg/min in /kg/day concentrated PN
in ml/kg/day in ml/kg/day
10 4.4 0.8 0.3 6.6
20 8.8 1.5 0.5 13.2
30 13.2 2.3 0.8 19.8
40 17.6 3.1 1.0 26.4
50 22.0 3.8 1.3 33.0
60 26.4 4.6 1.5 39.6
70 30.8 5.3 1.8 46.2
80 35.2 6.1 2.0 52.8
90 39.6 6.9 2.3 59.4
100 44.0 7.6 2.5 66.0
110 48.4 8.4 2.8 72.6
120 52.8 9.2 3.0 79.2
130 57.1 9.9 3.3 85.8
136.7 60.1 10.4 3.5 90.2
140 61.5 10.7 3.5 92.4
150 65.9 11.5 3.8 99.0
156.3 68.7 11.9 4.0 103.2
Recommended
Acceptable
Not recommended (in majority of cases)
BOLD Target Range
Establishing Infusion Rate
4
Department of Neonatology, BSUH, 2011
no reviews yet
Please Login to review.