194x Filetype PDF File size 0.21 MB Source: www.meddean.luc.edu
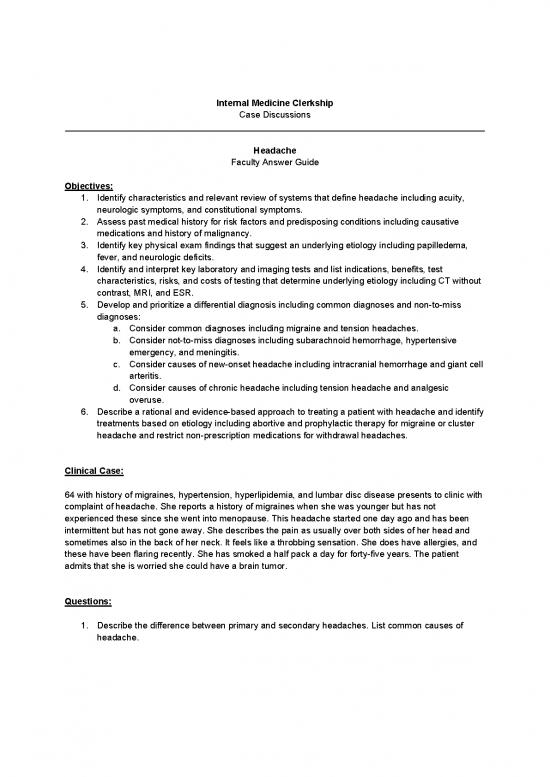
Internal Medicine Clerkship
Case Discussions
____________________________________________________________________________________
Headache
Faculty Answer Guide
Objectives:
1. Identify characteristics and relevant review of systems that define headache including acuity,
neurologic symptoms, and constitutional symptoms.
2. Assess past medical history for risk factors and predisposing conditions including causative
medications and history of malignancy.
3. Identify key physical exam findings that suggest an underlying etiology including papilledema,
fever, and neurologic deficits.
4. Identify and interpret key laboratory and imaging tests and list indications, benefits, test
characteristics, risks, and costs of testing that determine underlying etiology including CT without
contrast, MRI, and ESR.
5. Develop and prioritize a differential diagnosis including common diagnoses and non-to-miss
diagnoses:
a. Consider common diagnoses including migraine and tension headaches.
b. Consider not-to-miss diagnoses including subarachnoid hemorrhage, hypertensive
emergency, and meningitis.
c. Consider causes of new-onset headache including intracranial hemorrhage and giant cell
arteritis.
d. Consider causes of chronic headache including tension headache and analgesic
overuse.
6. Describe a rational and evidence-based approach to treating a patient with headache and identify
treatments based on etiology including abortive and prophylactic therapy for migraine or cluster
headache and restrict non-prescription medications for withdrawal headaches.
Clinical Case:
64 with history of migraines, hypertension, hyperlipidemia, and lumbar disc disease presents to clinic with
complaint of headache. She reports a history of migraines when she was younger but has not
experienced these since she went into menopause. This headache started one day ago and has been
intermittent but has not gone away. She describes the pain as usually over both sides of her head and
sometimes also in the back of her neck. It feels like a throbbing sensation. She does have allergies, and
these have been flaring recently. She has smoked a half pack a day for forty-five years. The patient
admits that she is worried she could have a brain tumor.
Questions:
1. Describe the difference between primary and secondary headaches. List common causes of
headache.
The International Headache Society characterizes primary headaches as those in which
the headache is the disorder itself, whereas secondary headaches are exogenous
disorders. Common causes and frequency are noted in the table below:
2. What other questions would you ask to help differentiate a serious from a more benign new onset
headache?
Worrisome historical features include the following: sudden-onset, first severe headache,
“worst” headache ever, vomiting that precedes the headache, subacute worsening over
days or weeks, pain induced by bending/lifting/coughing, pain that disturbs sleep or
presents immediately upon awakening, known systemic illness, onset after age 55, and
fever or unexplained systemic signs.
3. Given her history of migraines, what are other typical signs and symptoms of migraines you may
ask her about? What are the typical phases of a migraine?
Typical migraines are episodic and may be associated with sensitivity to light, sound, or
movement. Nausea and vomiting frequently accompany the headache. Other symptoms
include lightheadedness, scalp tenderness, vertigo, paresthesias, and visual disturbances.
Less commonly patients may experience loss of consciousness, diarrhea, syncope,
seizure, and confusion.
A migraine usually has three phases: prodrome, headache, and postdrome phase. About
25% of patients also describe a fourth phase which is the aura phase.
4. How are acute migraines typically treated? What are prophylactic treatments for chronic
migraines? What are non-pharmacologic strategies for treatment?
Patients should be instructed to keep a headache journal to try to identify triggers.
Common triggers include alcohol, caffeine, excess stress, poor sleep, and other dietary
triggers. Regular exercise and sleep, a healthy diet, and stress reduction measures may
help as well. These measures are unlikely to prevent all migraines but may be used as an
adjunct to pharmacologic approaches.
Acute migraines that are mild can be treated with oral medications including simple
analgesics (i.e., Excedrin Migraine, which includes acetaminophen, aspirin, and caffeine),
nsaids (i.e., naproxen, ibuprofen, and diclofenac), 5HT receptor antagonists (i.e.,
ergotamine and triptans), and dopamine receptor antagonist (i.e., metoclopramide and
chlorpromazine). These medications should be started as soon as possible after the onset
of the attack. More severe attacks may require parenteral medications.
Prophylactic treatment for chronic migraines includes beta-blockers (typically
propranolol), antidepressants (including amitriptyline, nortriptyline, and venlafaxine),
anticonvulsants (including topiramate and valproate). Newer therapies include single
pulse transcranial magnetic stimulation and botulin toxin injections.
5. What areas of your physical exam would you focus on?
Vitals are critical to make sure the patient is not very hypertensive, febrile, or hypoxic
which could all contribute to headaches. A complete neurologic exam should be
performed including a fundoscopic exam to assess for papilledema. You should also
assess for local tenderness in the area of the temporal artery or over the sinuses.
Physical Exam:
BP 147/89 HR 90 RR 18 O2 sat: 99% BMI 32
HEENT is normal and negative for papilledema, no tenderness over the frontal and maxillary sinuses
Heart, lungs, abdomen are normal
Neuro exam is unremarkable except for 1+ patellar reflexes bilaterally. The patient is reporting
disequilibrium with getting on and off the table and is having trouble finding her words during the
conversation.
Questions:
6. What is your primary concern at this point and what would you do for the patient?
Given her age, acuity of the headache, vascular risk factors, and some worrisome
symptoms including disequilibrium and word finding issues, she should be referred to the
emergency department for an emergent CT head to rule out an intracranial or
subarachnoid hemorrhage.
7. If the patient was febrile on exam what might else you be worried about? Are there additional
physical exam findings you would look for?
A fever would make you more concerned for an underlying systemic infection. Sinusitis in
light of her recent allergies could be considered. She should be asked about other upper
respiratory symptoms as well. Meningitis is possible, and if you were worried about this
you should look for evidence of nuchal rigidity as well as assess for the Kernig’s and
Brudzinski’s signs on exam. If meningitis was high on the differential, a lumbar puncture
should be considered.
8. How would you respond to the patient’s concern that she could have a brain tumor as the cause
of her symptoms?
Many patients express this concern but 0.1% of headaches are related to brain tumors.
She does have a significant smoking history and non-small cell lung cancer has a
tendency to metastasize to the brain, so this is still a possibility though less likely at this
point.
The patient’s CT brain is negative. Her basic laboratory evaluation, chest x-ray, and EKG are also
negative. She is given a dose of ketorolac with improvement and is sent home.
Three days later she returns to clinic with the same headache complaint. She is also describing some
pain in her neck and shoulders but thinks this is related to lying in the hospital bed in the emergency
room. In addition, she thinks she has noticed some intermittent blurry vision which she attributes to not
sleeping well due to the headache.
Questions:
9. Do her current symptoms suggest a different etiology of her headache at this point?
Given the persistent headache and now vision complaint and upper extremity pain,
temporal arteritis must be on the differential. Temporal arteritis is often seen in
conjunction with polymyalgia rheumatica which can cause shoulder and hip girdle pain. It
is quite feasible that these are simple muscular complaints, but the diagnosis of temporal
arteritis cannot be missed as it can lead to permanent blindness if not treated in a timely
and appropriate fashion.
10. What tests would you order if you were worried about temporal arteritis? Discuss the sensitivity,
specificity, and likelihood ratios of these tests. How would you treat her if this condition was high
on your differential?
If concerned about temporal arteritis you may consider an ESR, temporal artery
ultrasound, or temporal biopsy. The sensitivity of the ESR is 95%, so it can be used to rule
out temporal arteritis if negative (because it is almost always elevated in temporal
arteritis). For an ESR > 50, the LR+ is 1.2 and LR- 0.35; and for an ESR > 100 the LR+ is 1.9
and LR- is 0.08. Temporal artery ultrasound is often considered as a diagnostic tool as it is
non-invasive and low risk, but most studies have found this ultrasound to be insensitive
and not specific enough to avoid biopsy. A temporal artery biopsy is the gold standard for
diagnosis and should be done as soon as possible once the diagnosis is suspected.
no reviews yet
Please Login to review.